As a healthcare provider, you understand the importance of obtaining prior authorization (PA) for certain medical treatments and procedures. Allwell, a leading health insurance provider, requires prior authorization for specific services to ensure that patients receive necessary and cost-effective care. In this article, we will guide you through the 3 easy steps to complete the Allwell prior auth form, making the process smoother and more efficient for you and your patients.

Step 1: Determine If Prior Authorization Is Required
Before starting the prior authorization process, it's essential to determine if PA is required for the specific service or treatment you are recommending for your patient. Allwell provides a list of services that require prior authorization on their website. You can also contact Allwell's customer service department to confirm if PA is needed.
To determine if prior authorization is required, follow these steps:
- Check Allwell's website for the most up-to-date list of services that require prior authorization.
- Verify the patient's benefits and coverage to ensure that the service is covered under their plan.
- Review the patient's medical history to determine if the service is medically necessary.
Benefits of Determining Prior Authorization Requirements
Determining if prior authorization is required before starting the process can save time and reduce delays in patient care. By verifying the requirements upfront, you can:
- Avoid unnecessary paperwork and administrative tasks.
- Ensure that patients receive timely and necessary care.
- Reduce the risk of denied claims and subsequent appeals.

Step 2: Gather Required Documentation and Information
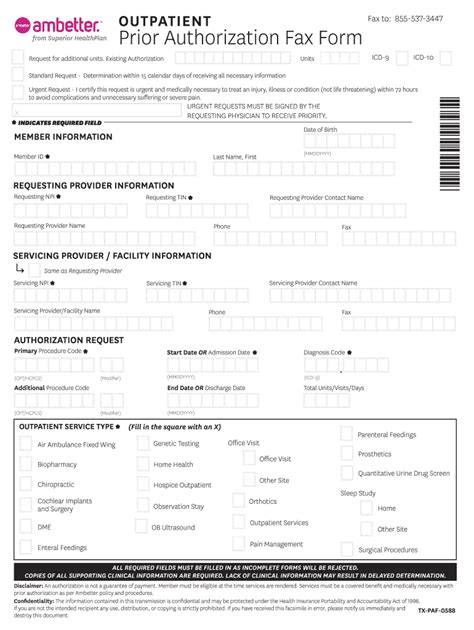
Once you have determined that prior authorization is required, gather all necessary documentation and information to complete the Allwell prior auth form. The required documents and information may vary depending on the specific service or treatment, but typically include:
- Patient demographics and contact information.
- Patient's medical history, including relevant test results and diagnoses.
- Detailed description of the service or treatment being requested.
- Supporting documentation, such as medical records and test results.
To ensure that you have all necessary documentation and information, follow these steps:
- Review the patient's medical records to gather relevant information.
- Obtain any additional documentation or test results required to support the request.
- Verify the patient's benefits and coverage to ensure that the service is covered under their plan.
Importance of Accurate and Complete Documentation
Accurate and complete documentation is crucial for a successful prior authorization request. By providing all necessary documentation and information, you can:
- Ensure that the request is processed efficiently and effectively.
- Reduce the risk of delays or denials due to incomplete or inaccurate information.
- Demonstrate the medical necessity of the service or treatment.

Step 3: Complete and Submit the Allwell Prior Auth Form
Once you have gathered all necessary documentation and information, complete and submit the Allwell prior auth form. The form can be found on Allwell's website or by contacting their customer service department.
To complete and submit the form, follow these steps:
- Fill out the form accurately and completely, including all required documentation and information.
- Review the form for accuracy and completeness before submitting.
- Submit the form via fax, email, or online portal, as specified by Allwell.
Tips for Successful Prior Authorization Submission
To ensure a successful prior authorization submission, follow these tips:
- Verify that all required documentation and information is included.
- Ensure that the form is complete and accurate to avoid delays or denials.
- Submit the form in a timely manner to avoid delays in patient care.

By following these 3 easy steps, you can efficiently and effectively complete the Allwell prior auth form, ensuring that your patients receive necessary and timely care. Remember to determine if prior authorization is required, gather all necessary documentation and information, and complete and submit the form accurately and completely.
We hope this article has been helpful in guiding you through the Allwell prior auth form completion process. If you have any questions or concerns, please don't hesitate to reach out.
What is prior authorization, and why is it required?
+Prior authorization is a process used by health insurance providers to determine if a specific service or treatment is medically necessary and covered under a patient's plan. It is required to ensure that patients receive necessary and cost-effective care.
How do I determine if prior authorization is required for a specific service or treatment?
+You can determine if prior authorization is required by checking Allwell's website for the most up-to-date list of services that require prior authorization, verifying the patient's benefits and coverage, and reviewing the patient's medical history.
What documentation and information is required to complete the Allwell prior auth form?
+The required documentation and information may vary depending on the specific service or treatment, but typically includes patient demographics and contact information, patient's medical history, detailed description of the service or treatment being requested, and supporting documentation.