Navigating the complexities of healthcare and insurance can be daunting, especially when it comes to accessing the medications you need. One crucial aspect of this process is the prior authorization form, a document that your healthcare provider must submit to your insurance company to obtain approval for certain treatments or medications. For individuals insured through Molina Healthcare, understanding the Molina Medication Prior Authorization Form is essential. Here, we delve into five key facts about this form to help you better understand the process and ensure you receive the care you require.

Understanding Prior Authorization
Prior authorization is a process used by health insurance companies to determine if a specific treatment or medication is medically necessary and will be covered under your insurance plan. It's essentially a pre-approval process that your healthcare provider must initiate before prescribing certain medications, especially those that are costly, have potential side effects, or are used to treat conditions that require close monitoring.
Why is Prior Authorization Necessary?
While it may seem like an extra hurdle, prior authorization is designed to ensure that patients receive safe and effective treatments. It allows insurance companies to assess whether a medication is appropriate for your condition and whether there are other, more cost-effective options available. This process can also help prevent unnecessary side effects and ensure that patients are aware of all their treatment options.
The Molina Medication Prior Authorization Form
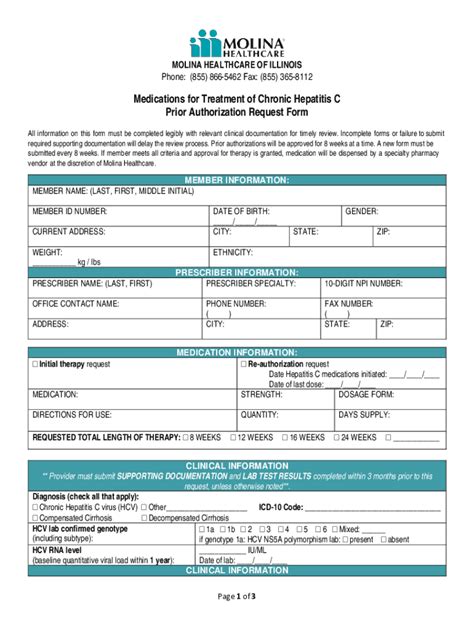
The Molina Medication Prior Authorization Form is a specific document that healthcare providers must complete and submit to Molina Healthcare for review. This form typically requires detailed information about the patient's condition, the medication being requested, and the clinical rationale for its use. The form is usually submitted electronically or by fax, and the review process can take several days to a few weeks, depending on the complexity of the request.

Key Information Required on the Form
To expedite the review process, it's essential that the Molina Medication Prior Authorization Form is completed accurately and thoroughly. Key information typically includes:
- Patient demographics and insurance information
- Detailed diagnosis and medical history related to the condition being treated
- Specific medication information, including dosage and frequency
- Clinical rationale for the medication, including any relevant medical literature or guidelines
- Information about previous treatments or medications tried
Steps to Complete the Prior Authorization Process
While the prior authorization process can seem daunting, understanding the steps involved can help streamline the experience. Here's a general overview of what to expect:
-
Consultation with Your Healthcare Provider: Discuss your treatment options with your healthcare provider, who will determine if a prior authorization is necessary for your medication.
-
Completion of the Prior Authorization Form: Your healthcare provider will complete the Molina Medication Prior Authorization Form with the required information.
-
Submission of the Form: The completed form is submitted to Molina Healthcare for review.
-
Review and Determination: Molina Healthcare reviews the request, which may involve verifying the information provided or requesting additional documentation.
-
Notification of Approval or Denial: You and your healthcare provider are notified of the decision. If approved, you can proceed with the prescribed medication. If denied, you may be able to appeal the decision.

Appealing a Denied Request
If your prior authorization request is denied, you have the right to appeal the decision. This involves submitting an appeal form and providing additional information or justification for why the medication is medically necessary. The appeal process is typically outlined in the denial notification and may involve several levels of review.
Importance of Understanding Your Insurance Coverage
Navigating the healthcare system requires a clear understanding of your insurance coverage, including what is covered and what requires prior authorization. Taking the time to review your insurance policy and asking questions can help prevent surprises and ensure that you receive the care you need without unnecessary delays.

Tips for a Smooth Prior Authorization Process
To minimize delays and ensure a smooth prior authorization process:
- Ensure your healthcare provider submits the form with complete and accurate information.
- Allow sufficient time for the review process.
- Stay informed about your insurance coverage and any changes that may affect your benefits.
- Don't hesitate to ask questions or seek clarification from your healthcare provider or insurance company.
Conclusion: Empowering Your Healthcare Journey
The Molina Medication Prior Authorization Form is a critical document in your healthcare journey, designed to ensure that you receive the right treatment while managing healthcare costs. By understanding the process and requirements involved, you can navigate the system more effectively and ensure that you get the care you need. Whether you're dealing with a chronic condition or facing a new diagnosis, being informed is key to making the best decisions about your health.
We invite you to share your experiences or ask questions about the prior authorization process in the comments below. Your insights can help others navigate this complex aspect of healthcare.
What is prior authorization, and why is it necessary?
+Prior authorization is a process used by health insurance companies to determine if a specific treatment or medication is medically necessary and will be covered under your insurance plan. It's necessary to ensure that patients receive safe and effective treatments, prevent unnecessary side effects, and explore more cost-effective options.
How long does the prior authorization process typically take?
+The review process can take several days to a few weeks, depending on the complexity of the request and the efficiency of the healthcare provider and insurance company.
Can I appeal a denied prior authorization request?
+Yes, if your prior authorization request is denied, you have the right to appeal the decision. This involves submitting an appeal form and providing additional information or justification for why the medication is medically necessary.