BlueCross BlueShield of Tennessee (BCBST) is one of the largest health insurance providers in the state, offering a range of plans to individuals, families, and employers. One of the essential processes in managing healthcare costs and ensuring that patients receive necessary treatments is prior authorization. In this article, we will delve into the world of prior authorization, focusing on the BCBST Tennessee prior authorization form, and provide a step-by-step guide on how to navigate this process.
Understanding Prior Authorization
Prior authorization, also known as pre-authorization or pre-certification, is a process used by health insurance providers to determine whether a specific treatment, medication, or service is medically necessary and covered under a patient's insurance plan. This process helps to prevent unnecessary medical procedures, reduce healthcare costs, and ensure that patients receive the most effective treatments.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- It helps to control healthcare costs by preventing unnecessary procedures and treatments.
- It ensures that patients receive the most effective treatments, reducing the risk of complications and improving health outcomes.
- It enables healthcare providers to communicate with insurance companies, ensuring that patients receive the necessary care without unexpected costs.
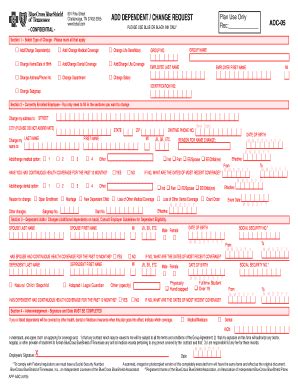
The BCBST Tennessee Prior Authorization Form
The BCBST Tennessee prior authorization form is a document used by healthcare providers to request prior authorization for specific treatments, medications, or services. The form typically includes the following information:
- Patient demographics and insurance information
- Treatment or service details, including the procedure code and description
- Medical necessity justification, including diagnosis and treatment plan
- Prescriber information and signature
Step-by-Step Guide to Completing the BCBST Tennessee Prior Authorization Form
Completing the BCBST Tennessee prior authorization form requires attention to detail and accurate information. Here's a step-by-step guide to help you navigate the process:

- Gather necessary information: Before starting the form, ensure you have the following information:
- Patient demographics, including name, date of birth, and insurance ID number
- Treatment or service details, including procedure code and description
- Medical necessity justification, including diagnosis and treatment plan
- Prescriber information, including name, title, and contact details
- Download the form: Visit the BCBST Tennessee website to download the prior authorization form. You can also contact the BCBST Tennessee customer service department to request a copy of the form.
- Complete the patient demographics section: Fill in the patient's name, date of birth, insurance ID number, and other relevant demographics.
- Enter treatment or service details: Provide the procedure code, description, and other relevant details about the treatment or service being requested.
- Justify medical necessity: Explain the medical necessity of the treatment or service, including the diagnosis and treatment plan.
- Provide prescriber information: Enter the prescriber's name, title, and contact details.
- Sign and date the form: Sign and date the form, ensuring that the prescriber has authorized the request.
- Submit the form: Fax or mail the completed form to BCBST Tennessee, following the instructions provided on the form.
Tips for Submitting the BCBST Tennessee Prior Authorization Form
To ensure a smooth prior authorization process, follow these tips:
- Verify patient eligibility and benefits before submitting the form.
- Ensure accurate and complete information, as incomplete forms may be delayed or denied.
- Use the correct form version, as outdated forms may not be accepted.
- Submit the form well in advance of the treatment or service date to avoid delays.
BCBST Tennessee Prior Authorization Form Requirements
BCBST Tennessee requires prior authorization for certain treatments, medications, and services. Some of the most common requirements include:
- Advanced imaging services, such as MRI and CT scans
- Biologic medications, such as injectables and infusions
- Durable medical equipment, such as wheelchairs and oxygen therapy
- Home health services, including skilled nursing and physical therapy
Common Mistakes to Avoid
When completing the BCBST Tennessee prior authorization form, avoid the following common mistakes:
- Incomplete or inaccurate information
- Using outdated forms or incorrect procedure codes
- Failing to justify medical necessity or provide supporting documentation
- Not signing and dating the form
Frequently Asked Questions
What is prior authorization?
+Prior authorization is a process used by health insurance providers to determine whether a specific treatment, medication, or service is medically necessary and covered under a patient's insurance plan.
Why do I need to complete a prior authorization form?
+You need to complete a prior authorization form to request approval for specific treatments, medications, or services. This helps to ensure that you receive the necessary care without unexpected costs.
How long does the prior authorization process take?
+The prior authorization process typically takes 24-48 hours, but may vary depending on the complexity of the request and the availability of necessary information.
Conclusion
The BCBST Tennessee prior authorization form is an essential document used to request prior authorization for specific treatments, medications, or services. By following the step-by-step guide and tips outlined in this article, you can ensure a smooth prior authorization process and help your patients receive the necessary care without unexpected costs.
What's Next?
If you have any questions or concerns about the BCBST Tennessee prior authorization form or process, please don't hesitate to reach out to our team. We're here to help you navigate the complexities of healthcare and ensure that your patients receive the best possible care.
Share Your Thoughts
Have you experienced any challenges with the prior authorization process? Share your thoughts and experiences in the comments below. We'd love to hear from you and help you find solutions to any challenges you may be facing.