The complexities of healthcare paperwork can be overwhelming, especially when it comes to Medicaid prior authorization forms. Meridian Medicaid, a leading healthcare provider, requires prior authorization for certain medical procedures and treatments to ensure that patients receive necessary and cost-effective care. In this article, we will break down the Meridian Medicaid prior auth form into 5 easy steps, making it more manageable for healthcare providers and patients alike.
Understanding the Importance of Prior Authorization
Prior authorization is a crucial step in the healthcare process, ensuring that patients receive necessary and medically appropriate care while also controlling healthcare costs. By requiring prior authorization, Meridian Medicaid can review medical requests to determine if they meet specific criteria, reducing unnecessary procedures and minimizing waste.
Step 1: Gather Required Information

Before starting the Meridian Medicaid prior auth form, it's essential to gather all required information. This includes:
- Patient demographics and contact information
- Medical records and relevant test results
- Prescription information and medication history
- Treatment plans and medical necessity documentation
Having all necessary information readily available will streamline the prior authorization process, reducing delays and increasing the likelihood of approval.
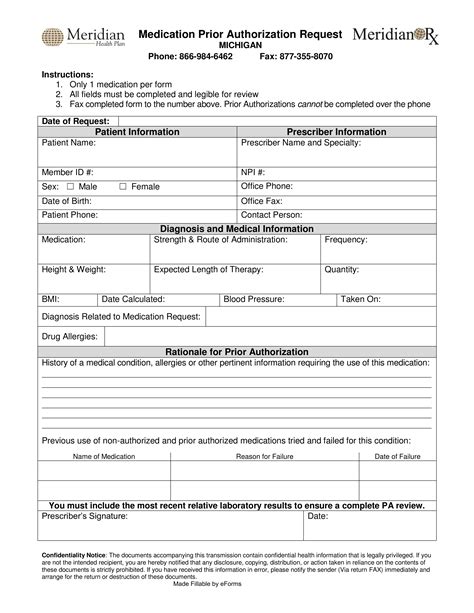
Step 2: Complete the Prior Auth Form
Meridian Medicaid Prior Auth Form: A Step-by-Step Guide

The Meridian Medicaid prior auth form is a straightforward document that requires specific information to process the request. The form typically includes sections for:
- Patient and provider information
- Procedure or treatment details
- Medical necessity documentation
- Supporting documentation and attachments
When completing the form, be sure to:
- Fill out all required fields accurately and completely
- Attach supporting documentation, such as medical records and test results
- Clearly explain the medical necessity of the requested procedure or treatment
Step 3: Submit the Prior Auth Request
Submission Options and Timelines
Once the prior auth form is complete, it's time to submit the request to Meridian Medicaid. Submission options may vary depending on the provider's preference and Meridian Medicaid's policies. Common submission methods include:
- Fax: 555-555-5555
- Email:
- Online portal:
Be sure to submit the request well in advance of the scheduled procedure or treatment to allow sufficient time for processing and review.
Step 4: Track and Follow Up on the Prior Auth Request
Understanding the Review Process and Timeline
After submitting the prior auth request, it's essential to track and follow up on the status. Meridian Medicaid typically reviews prior auth requests within 3-5 business days, but this timeline may vary depending on the complexity of the request.
Providers can:
- Check the online portal for updates on the request status
- Contact Meridian Medicaid's prior auth department via phone or email to inquire about the status
- Follow up with additional documentation or information as requested by Meridian Medicaid
Step 5: Receive and Respond to the Prior Auth Determination
Understanding the Determination and Next Steps
Once Meridian Medicaid has reviewed the prior auth request, they will issue a determination letter indicating approval, denial, or additional information required. Providers should:
- Review the determination letter carefully and understand the reasons for the decision
- Respond to any requests for additional information or documentation
- Inform the patient of the determination and next steps
By following these 5 easy steps, healthcare providers and patients can navigate the Meridian Medicaid prior auth form process with confidence, ensuring that necessary care is received in a timely and efficient manner.
Conclusion: Simplifying the Prior Auth Process
In conclusion, the Meridian Medicaid prior auth form process can seem daunting, but by breaking it down into manageable steps, healthcare providers and patients can ensure a smoother experience. By understanding the importance of prior authorization, gathering required information, completing the form accurately, submitting the request, tracking and following up, and responding to the determination, everyone involved can work together to provide high-quality, cost-effective care.
FAQ Section
What is prior authorization, and why is it required?
+Prior authorization is a process where Meridian Medicaid reviews medical requests to ensure that patients receive necessary and cost-effective care. It's required to control healthcare costs and reduce unnecessary procedures.
How long does the prior auth review process typically take?
+The prior auth review process typically takes 3-5 business days, but this timeline may vary depending on the complexity of the request.
What happens if my prior auth request is denied?
+If your prior auth request is denied, you will receive a determination letter explaining the reasons for the decision. You can respond to the denial by providing additional information or documentation, or by appealing the decision.