In today's healthcare landscape, prior authorization has become a crucial step in ensuring that patients receive the necessary medical treatments while also controlling healthcare costs. For FEPBlue (Federal Employee Program Blue Cross Blue Shield) beneficiaries, navigating the prior authorization process can be overwhelming. In this article, we will outline the 5 steps to FEPBlue prior authorization form approval, providing a comprehensive guide to help you successfully navigate this process.

Understanding FEPBlue Prior Authorization
Before diving into the steps, it's essential to understand what prior authorization entails. Prior authorization is a process where a healthcare provider must obtain approval from FEPBlue before performing a specific medical treatment or prescribing a particular medication. This ensures that the treatment is medically necessary and meets FEPBlue's coverage guidelines.
Step 1: Review FEPBlue's Prior Authorization Requirements
The first step in the prior authorization process is to review FEPBlue's requirements. This includes understanding which medical treatments or medications require prior authorization, as well as the necessary documentation and information needed for approval. You can find this information on FEPBlue's website or by contacting their customer service department.
Step 2: Gather Required Documentation and Information
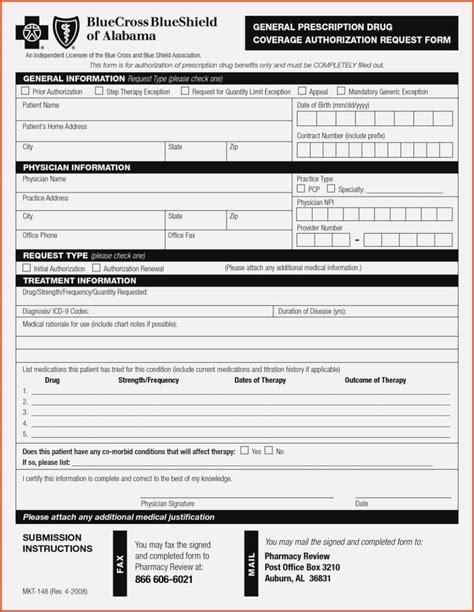
Once you understand FEPBlue's prior authorization requirements, the next step is to gather the necessary documentation and information. This may include:
- Patient's medical history and diagnosis
- Treatment plan and medication list
- Supporting medical records and test results
- Patient's demographic and insurance information

Step 3: Submit the Prior Authorization Request
After gathering the necessary documentation and information, the next step is to submit the prior authorization request to FEPBlue. This can be done online, by phone, or by mail, depending on FEPBlue's requirements. Make sure to submit the request in a timely manner, as delays can impact the approval process.
Tips for Submitting a Successful Prior Authorization Request
- Ensure all required documentation and information is included
- Double-check for accuracy and completeness
- Submit the request well in advance of the scheduled treatment or medication start date
Step 4: Follow-up on the Prior Authorization Request
After submitting the prior authorization request, it's essential to follow up with FEPBlue to ensure that the request is being processed. This can be done by contacting FEPBlue's customer service department or checking the status online. Be prepared to provide additional information or clarification if needed.

Step 5: Receive and Review the Prior Authorization Decision
The final step is to receive and review the prior authorization decision from FEPBlue. If approved, ensure that you understand the terms and conditions of the approval, including any limitations or restrictions. If denied, review the denial reason and consider appealing the decision if necessary.
Conclusion
Navigating the FEPBlue prior authorization process can be complex, but by following these 5 steps, you can increase the chances of a successful approval. Remember to review FEPBlue's requirements, gather necessary documentation and information, submit the request in a timely manner, follow up on the request, and review the prior authorization decision carefully.

We hope this article has provided you with a comprehensive guide to FEPBlue prior authorization form approval. If you have any further questions or concerns, please don't hesitate to reach out to us.
What is prior authorization, and why is it required?
+Prior authorization is a process where a healthcare provider must obtain approval from FEPBlue before performing a specific medical treatment or prescribing a particular medication. This ensures that the treatment is medically necessary and meets FEPBlue's coverage guidelines.
How long does the prior authorization process take?
+The prior authorization process typically takes 1-3 business days, but can take longer in some cases. It's essential to submit the request in a timely manner to avoid delays.