In the healthcare industry, navigating the complexities of prior authorization forms can be a daunting task for medical professionals and patients alike. The Epiphany Rx Prior Authorization Form is one such document that plays a crucial role in ensuring that patients receive the necessary medication while also controlling healthcare costs. In this article, we will delve into the intricacies of the Epiphany Rx Prior Authorization Form, providing a comprehensive, step-by-step guide to help healthcare providers and patients alike.
The Epiphany Rx Prior Authorization Form is a crucial document that facilitates communication between healthcare providers, patients, and insurance companies. Its primary purpose is to obtain pre-approval for medication or treatment, ensuring that patients receive the necessary care while also managing healthcare costs. By understanding the intricacies of this form, healthcare providers can streamline the prior authorization process, reducing delays and ensuring that patients receive timely treatment.
Understanding the Epiphany Rx Prior Authorization Form

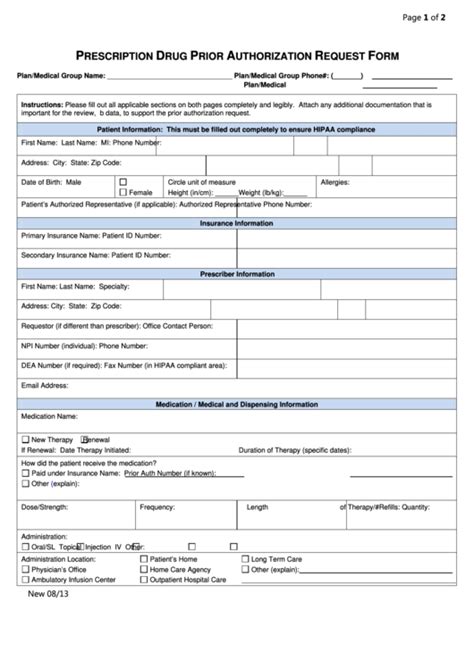
The Epiphany Rx Prior Authorization Form typically consists of several sections, each designed to capture specific information about the patient, medication, and treatment plan. The form may vary depending on the insurance provider and the specific medication or treatment being requested.
Section 1: Patient Information
The first section of the form typically requires patient demographic information, including name, date of birth, and contact details. This information is essential for identifying the patient and verifying their eligibility for the requested medication or treatment.Section 2: Medication Information
This section requires detailed information about the medication or treatment being requested, including the medication name, dosage, and frequency. The healthcare provider must also indicate the diagnosis or condition being treated, as well as any relevant medical history.Section 3: Clinical Information
The clinical information section requires the healthcare provider to provide additional context about the patient's condition, including any relevant laboratory results, medical imaging, or other diagnostic tests.Section 4: Treatment Plan
This section requires the healthcare provider to outline the treatment plan, including the expected duration of treatment and any potential side effects or interactions.Section 5: Supporting Documentation
The final section requires the healthcare provider to attach any supporting documentation, including medical records, test results, or other relevant information.Completing the Epiphany Rx Prior Authorization Form

Completing the Epiphany Rx Prior Authorization Form requires careful attention to detail and a thorough understanding of the patient's medical history and treatment plan. Here are some tips to help healthcare providers complete the form accurately:
- Ensure that all patient demographic information is accurate and up-to-date.
- Clearly indicate the diagnosis or condition being treated, as well as any relevant medical history.
- Provide detailed information about the medication or treatment being requested, including dosage and frequency.
- Attach any supporting documentation, including medical records or test results.
- Review the form carefully to ensure that all sections are complete and accurate.
Submitting the Epiphany Rx Prior Authorization Form

Once the Epiphany Rx Prior Authorization Form is complete, healthcare providers can submit it to the insurance company for review. The submission process typically involves faxing or emailing the form to the insurance company, along with any supporting documentation.
- Ensure that the form is submitted to the correct insurance company and department.
- Verify that all required documentation is attached, including medical records and test results.
- Follow up with the insurance company to confirm receipt of the form and to determine the status of the prior authorization request.
Tracking the Status of the Prior Authorization Request
Once the Epiphany Rx Prior Authorization Form is submitted, healthcare providers can track the status of the prior authorization request by contacting the insurance company. This can typically be done by phone, email, or through an online portal.
- Contact the insurance company to confirm receipt of the form and to determine the status of the prior authorization request.
- Verify that all required documentation has been received and is being reviewed.
- Follow up with the insurance company to determine the outcome of the prior authorization request.
Appealing a Denied Prior Authorization Request

If the prior authorization request is denied, healthcare providers can appeal the decision by submitting additional documentation or providing further clarification.
- Review the denial letter to understand the reason for the denial.
- Gather additional documentation or information to support the prior authorization request.
- Submit the appeal to the insurance company, along with any supporting documentation.
By understanding the intricacies of the Epiphany Rx Prior Authorization Form and following the steps outlined in this guide, healthcare providers can streamline the prior authorization process, reducing delays and ensuring that patients receive timely treatment. Remember to complete the form accurately, submit it to the correct insurance company, and track the status of the prior authorization request to ensure a smooth and efficient process.
What is the purpose of the Epiphany Rx Prior Authorization Form?
+The Epiphany Rx Prior Authorization Form is used to obtain pre-approval for medication or treatment, ensuring that patients receive the necessary care while also managing healthcare costs.
How do I complete the Epiphany Rx Prior Authorization Form?
+Complete the form carefully, ensuring that all patient demographic information is accurate and up-to-date. Clearly indicate the diagnosis or condition being treated, as well as any relevant medical history. Provide detailed information about the medication or treatment being requested, including dosage and frequency. Attach any supporting documentation, including medical records or test results.
How do I track the status of the prior authorization request?
+Contact the insurance company to confirm receipt of the form and to determine the status of the prior authorization request. Verify that all required documentation has been received and is being reviewed. Follow up with the insurance company to determine the outcome of the prior authorization request.