As a healthcare provider, managing patient care can be a complex and time-consuming process. One crucial aspect of this process is navigating the prior authorization requirements for insurance providers. In this article, we will focus on the EmblemHealth prior authorization form, a crucial document for healthcare providers to obtain approval for certain medical procedures, treatments, and medications.
Understanding the Importance of Prior Authorization
Prior authorization, also known as pre-certification or pre-authorization, is a process that requires healthcare providers to obtain approval from the insurance provider before administering specific medical treatments or services. This process helps ensure that patients receive medically necessary care while minimizing unnecessary costs. For healthcare providers, prior authorization is essential for avoiding denied claims, reducing administrative burdens, and maintaining a smooth workflow.

What is EmblemHealth Prior Authorization Form?
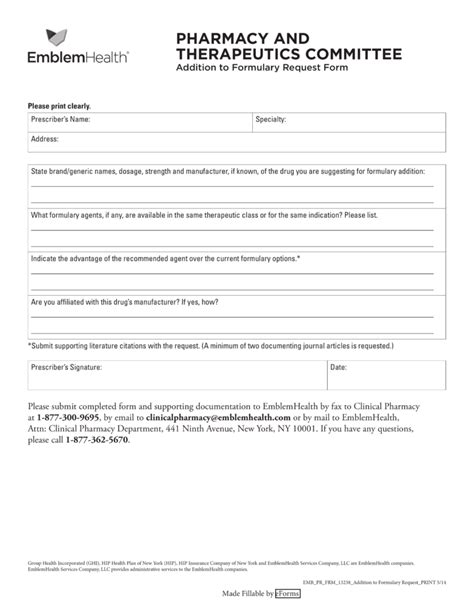
EmblemHealth is a health insurance provider that offers a range of plans for individuals, families, and businesses. The EmblemHealth prior authorization form is a document that healthcare providers must complete and submit to obtain approval for specific medical services, treatments, or medications. This form requires detailed information about the patient's condition, medical history, and the proposed treatment plan.
Why is EmblemHealth Prior Authorization Form Necessary?
The EmblemHealth prior authorization form is necessary to ensure that patients receive medically necessary care while minimizing unnecessary costs. By reviewing the form, EmblemHealth can determine whether the proposed treatment is consistent with their coverage policies and guidelines. This process helps prevent unnecessary procedures, reduces costs, and promotes efficient use of healthcare resources.
Step-by-Step Guide to Completing the EmblemHealth Prior Authorization Form
Completing the EmblemHealth prior authorization form requires attention to detail and accurate information. Here's a step-by-step guide to help healthcare providers navigate the process:
Step 1: Gather Patient Information
- Collect the patient's demographic information, including name, date of birth, and insurance ID number.
- Verify the patient's eligibility and coverage details.
Step 2: Determine the Type of Service or Treatment
- Identify the specific medical service, treatment, or medication requiring prior authorization.
- Ensure that the requested service is consistent with EmblemHealth's coverage policies and guidelines.
Step 3: Complete the Prior Authorization Form
- Download the EmblemHealth prior authorization form from the EmblemHealth website or access it through the online portal.
- Complete the form accurately, providing detailed information about the patient's condition, medical history, and the proposed treatment plan.
- Attach supporting documentation, such as medical records, test results, and treatment plans.
Step 4: Submit the Prior Authorization Form
- Submit the completed form to EmblemHealth via fax, email, or online portal.
- Ensure that the form is received by EmblemHealth within the required timeframe.

What Happens After Submitting the Prior Authorization Form?
After submitting the prior authorization form, EmblemHealth will review the request to determine whether the proposed treatment is medically necessary and consistent with their coverage policies and guidelines. The review process may take several days to several weeks, depending on the complexity of the request.
Possible Outcomes
- Approval: EmblemHealth approves the requested service or treatment, and the patient can proceed with the care.
- Denial: EmblemHealth denies the requested service or treatment, and the patient may appeal the decision.
- Additional Information Requested: EmblemHealth requests additional information or documentation to support the request.
Tips for Streamlining the Prior Authorization Process
- Familiarize yourself with EmblemHealth's prior authorization policies and guidelines.
- Ensure accurate and complete information on the prior authorization form.
- Submit the form well in advance of the proposed treatment date.
- Follow up with EmblemHealth to confirm receipt and review status.

Conclusion: Mastering the EmblemHealth Prior Authorization Form
Mastering the EmblemHealth prior authorization form requires attention to detail, accurate information, and a thorough understanding of the process. By following the step-by-step guide and tips outlined in this article, healthcare providers can streamline the prior authorization process, reduce administrative burdens, and ensure that patients receive the necessary care.
We encourage you to share your experiences and tips for navigating the prior authorization process in the comments section below. Your insights can help others improve their workflow and patient care.
What is the purpose of the EmblemHealth prior authorization form?
+The purpose of the EmblemHealth prior authorization form is to ensure that patients receive medically necessary care while minimizing unnecessary costs.
How long does the prior authorization process take?
+The prior authorization process may take several days to several weeks, depending on the complexity of the request.
What happens if EmblemHealth denies the prior authorization request?
+If EmblemHealth denies the prior authorization request, the patient may appeal the decision.