BCBS Michigan, also known as Blue Cross Blue Shield of Michigan, is a prominent health insurance provider in the state of Michigan. Like any health insurance company, BCBS Michigan has its own set of rules and procedures for handling provider appeals. If you're a healthcare provider in Michigan, it's essential to understand the BCBS Michigan provider appeal process to ensure that you're reimbursed fairly for the services you provide to patients.
The BCBS Michigan provider appeal form is a crucial document that you'll need to complete when appealing a claim denial or reimbursement decision. In this article, we'll provide a step-by-step guide on how to complete the form, along with some valuable tips and insights to help you navigate the appeal process successfully.
Understanding the BCBS Michigan Provider Appeal Process
Before we dive into the appeal form, let's take a brief look at the BCBS Michigan provider appeal process. The process typically involves the following steps:
- Initial Review: BCBS Michigan reviews your claim to determine whether it meets their reimbursement guidelines.
- Claim Denial: If your claim is denied, you'll receive a notification explaining the reason for the denial.
- Provider Appeal: You can appeal the denial by submitting a provider appeal form, along with supporting documentation.
- Appeal Review: BCBS Michigan reviews your appeal and may request additional information.
- Appeal Decision: You'll receive a decision on your appeal, which may be approved, denied, or partially approved.
Step-by-Step Guide to Completing the BCBS Michigan Provider Appeal Form
Now that we've covered the basics of the appeal process, let's move on to the BCBS Michigan provider appeal form. Here's a step-by-step guide to help you complete the form:
Step 1: Gather Required Information and Documents
Before you start filling out the form, make sure you have the following information and documents ready:
- Claim denial notification
- Patient's name and date of birth
- Claim number and date of service
- CPT/HCPCS codes and description of services provided
- Supporting documentation, such as medical records and test results

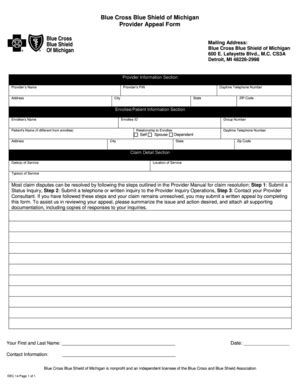
Step 2: Complete the Provider Information Section
The first section of the form requires you to provide your provider information, including:
- Your name and title
- Your practice name and address
- Your NPI number and taxonomy code
Step 3: Complete the Patient Information Section
The next section requires you to provide patient information, including:
- Patient's name and date of birth
- Patient's insurance ID number
Step 4: Complete the Claim Information Section
This section requires you to provide claim-specific information, including:
- Claim number and date of service
- CPT/HCPCS codes and description of services provided
- Billed amount and allowed amount
Step 5: Explain the Reason for the Appeal
In this section, you'll need to explain why you're appealing the claim denial. Be sure to provide a clear and concise explanation, including any relevant medical information or documentation.
Step 6: Attach Supporting Documentation
This is where you'll attach any supporting documentation, such as medical records, test results, or expert opinions.
Step 7: Sign and Date the Form
Finally, be sure to sign and date the form. This is an important step, as it verifies that you're the provider who's submitting the appeal.
Tips and Insights for a Successful Appeal
While the BCBS Michigan provider appeal form may seem straightforward, there are a few tips and insights to keep in mind to ensure a successful appeal:
- Be sure to submit the appeal form within the required timeframe (typically 180 days from the claim denial notification).
- Provide clear and concise explanations for the appeal, including any relevant medical information or documentation.
- Attach all supporting documentation, including medical records, test results, and expert opinions.
- Keep a copy of the appeal form and supporting documentation for your records.
Common Mistakes to Avoid
When completing the BCBS Michigan provider appeal form, there are a few common mistakes to avoid:
- Incomplete or inaccurate information
- Failure to attach supporting documentation
- Missing signature or date
- Submitting the appeal form outside of the required timeframe
By following these steps and tips, you can ensure a successful appeal and avoid common mistakes. Remember to stay organized, provide clear and concise explanations, and attach all supporting documentation.
Conclusion
The BCBS Michigan provider appeal form is an essential document for healthcare providers in Michigan who need to appeal a claim denial or reimbursement decision. By following the step-by-step guide outlined in this article, you can ensure a successful appeal and avoid common mistakes. Remember to stay organized, provide clear and concise explanations, and attach all supporting documentation. If you have any questions or concerns, don't hesitate to reach out to BCBS Michigan or a qualified healthcare consultant.
FAQ Section
What is the BCBS Michigan provider appeal form?
+The BCBS Michigan provider appeal form is a document that healthcare providers use to appeal a claim denial or reimbursement decision.
How do I submit the BCBS Michigan provider appeal form?
+You can submit the appeal form by mail, fax, or online through the BCBS Michigan provider portal.
What is the required timeframe for submitting the BCBS Michigan provider appeal form?
+The required timeframe for submitting the appeal form is typically 180 days from the claim denial notification.