Managing healthcare services can be a daunting task, especially when it comes to navigating the complexities of prior authorization. For HMSA (Hawaii Medical Service Association) members, understanding the prior authorization process is crucial to ensure smooth and hassle-free healthcare experiences. In this article, we will delve into the world of HMSA prior authorization, explaining its importance, benefits, and providing a step-by-step guide on how to complete the HMSA prior authorization form.

Prior authorization is a process used by healthcare payers, including HMSA, to evaluate the medical necessity of certain treatments, medications, or services before they are rendered. This process helps ensure that patients receive evidence-based care, reduces unnecessary healthcare spending, and promotes better health outcomes.
Benefits of HMSA Prior Authorization
Prior authorization offers numerous benefits for HMSA members, including:
- Cost savings: By ensuring that only medically necessary services are rendered, prior authorization can help reduce healthcare costs and lower out-of-pocket expenses for members.
- Improved health outcomes: Prior authorization encourages the use of evidence-based treatments and services, leading to better health outcomes and improved quality of life.
- Reduced administrative burden: HMSA's prior authorization process streamlines the approval process, reducing the administrative burden on healthcare providers and minimizing delays in care.
5 Easy Steps for HMSA Prior Authorization Form
Completing the HMSA prior authorization form can seem overwhelming, but breaking it down into smaller steps makes the process more manageable. Here's a step-by-step guide to help you navigate the HMSA prior authorization form:
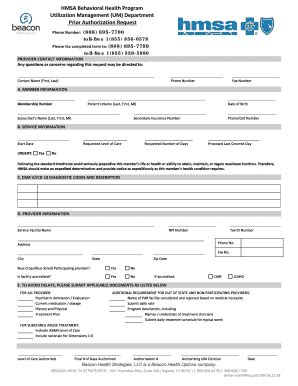
Step 1: Gather Required Information
Before starting the prior authorization process, gather all necessary information, including:
- Patient demographics and HMSA membership information
- Healthcare provider information and contact details
- Procedure or service codes (CPT/HCPCS)
- Diagnosis codes (ICD-10)
- Supporting medical documentation (e.g., medical records, test results)

Step 2: Choose the Correct Form
HMSA offers various prior authorization forms, depending on the type of service or treatment required. Select the correct form for your specific needs:
- HMSA Prior Authorization Request Form (for most services)
- HMSA Pharmacy Prior Authorization Form (for prescription medications)
- HMSA Durable Medical Equipment (DME) Prior Authorization Form (for DME services)
Step 3: Complete the Form
Carefully complete the selected form, ensuring that all required fields are filled in accurately and thoroughly. Attach supporting medical documentation as needed.

Step 4: Submit the Form
Submit the completed form and supporting documentation to HMSA via:
- Fax: (808) 948-6370
- Mail: HMSA, Prior Authorization Department, P.O. Box 860, Honolulu, HI 96808
- Online: HMSA's provider portal (for contracted providers)
Step 5: Follow Up
After submitting the prior authorization request, follow up with HMSA to confirm receipt and status:
- Call HMSA's Prior Authorization Department at (808) 948-6370
- Check the status online through HMSA's provider portal (for contracted providers)

By following these 5 easy steps, you'll be well on your way to successfully completing the HMSA prior authorization form and ensuring that your healthcare needs are met.
Tips for a Smooth Prior Authorization Process
To ensure a smooth prior authorization process, keep the following tips in mind:
- Verify HMSA coverage: Confirm that the requested service or treatment is covered under the patient's HMSA plan.
- Use correct codes: Accurately use CPT/HCPCS and ICD-10 codes to avoid delays or denials.
- Attach supporting documentation: Provide comprehensive medical documentation to support the prior authorization request.
- Submit requests timely: Submit prior authorization requests well in advance of the scheduled service or treatment.

By understanding the HMSA prior authorization process and following these simple steps, you'll be better equipped to navigate the complexities of healthcare and ensure that your patients receive the care they need.
If you have any questions or concerns about the HMSA prior authorization process, please don't hesitate to reach out. Share your experiences or ask questions in the comments below. Let's work together to make healthcare more accessible and efficient for everyone.
What is prior authorization?
+Prior authorization is a process used by healthcare payers to evaluate the medical necessity of certain treatments, medications, or services before they are rendered.
Why is prior authorization necessary?
+Prior authorization ensures that patients receive evidence-based care, reduces unnecessary healthcare spending, and promotes better health outcomes.
How long does the prior authorization process take?
+The prior authorization process typically takes 2-5 business days, but may vary depending on the complexity of the request and the speed of response from healthcare providers.