As a healthcare provider, navigating the complexities of prior authorization forms can be a daunting task. One of the most commonly used forms is the Aetna TMS Prior Auth Form. In this article, we will provide a simplified guide to help you understand the form and its requirements.
Prior authorization is a process used by health insurance companies to determine whether a specific treatment or service is medically necessary and covered under the patient's insurance plan. Aetna, one of the largest health insurance providers in the United States, requires healthcare providers to submit a prior auth form for certain treatments, including Transcranial Magnetic Stimulation (TMS).

The Aetna TMS Prior Auth Form is used to request approval for TMS treatment, which is a non-invasive brain stimulation therapy used to treat depression and other mental health conditions. In this section, we will break down the form and its requirements.
Understanding the Aetna TMS Prior Auth Form
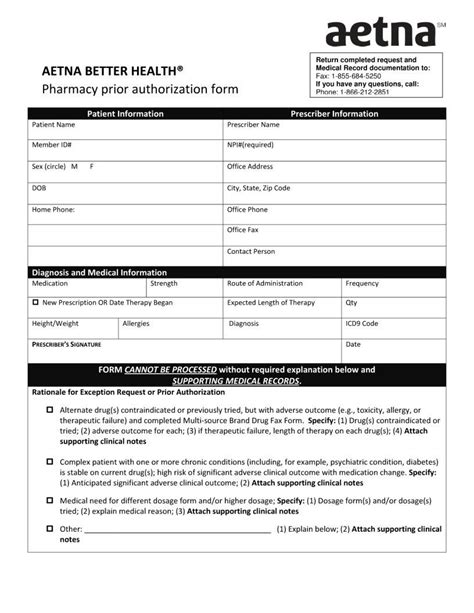
The Aetna TMS Prior Auth Form is a multi-page document that requires healthcare providers to submit detailed information about the patient's medical history, diagnosis, and treatment plan. The form is typically submitted electronically or by fax to Aetna's prior authorization department.

The form is divided into several sections, including:
- Patient information: This section requires healthcare providers to submit the patient's demographic information, including name, date of birth, and insurance identification number.
- Medical history: This section requires healthcare providers to submit the patient's medical history, including any previous diagnoses, treatments, and medications.
- Diagnosis: This section requires healthcare providers to submit the patient's diagnosis, including the ICD-10 code and a brief description of the condition.
- Treatment plan: This section requires healthcare providers to submit the treatment plan, including the type and frequency of TMS treatment.
Required Documents and Information
In addition to the completed prior auth form, Aetna requires healthcare providers to submit several supporting documents, including:
- Medical records: Healthcare providers must submit the patient's medical records, including any relevant test results, treatment plans, and progress notes.
- Prescription: Healthcare providers must submit a prescription for TMS treatment, including the type and frequency of treatment.
- Diagnostic reports: Healthcare providers must submit any diagnostic reports, including EEG or MRI results.

The Prior Auth Process
Once the prior auth form and supporting documents are submitted, Aetna's prior authorization department will review the request to determine whether the treatment is medically necessary and covered under the patient's insurance plan.
The prior auth process typically takes several days to several weeks, depending on the complexity of the request and the availability of information.

If the request is approved, Aetna will issue a prior authorization approval letter, which must be retained by the healthcare provider for billing and auditing purposes.
Denials and Appeals
If the request is denied, Aetna will issue a denial letter, which must be reviewed and appealed by the healthcare provider.
Healthcare providers can appeal the denial by submitting additional information or documentation to support the request.

Best Practices for Submitting the Aetna TMS Prior Auth Form
To ensure a smooth prior auth process, healthcare providers should follow these best practices:
- Submit complete and accurate information: Ensure that all required fields are completed and accurate to avoid delays or denials.
- Use clear and concise language: Use clear and concise language when describing the patient's medical history, diagnosis, and treatment plan.
- Submit supporting documents: Submit all required supporting documents, including medical records, prescriptions, and diagnostic reports.
- Follow up: Follow up with Aetna's prior authorization department to ensure that the request is processed in a timely manner.

Conclusion
The Aetna TMS Prior Auth Form is a complex document that requires healthcare providers to submit detailed information about the patient's medical history, diagnosis, and treatment plan. By following the best practices outlined in this article, healthcare providers can ensure a smooth prior auth process and reduce the risk of delays or denials.
We hope that this article has provided a simplified guide to the Aetna TMS Prior Auth Form and its requirements. If you have any questions or concerns, please do not hesitate to contact us.
What is the Aetna TMS Prior Auth Form?
+The Aetna TMS Prior Auth Form is a multi-page document that requires healthcare providers to submit detailed information about the patient's medical history, diagnosis, and treatment plan.
What is the purpose of the prior auth form?
+The purpose of the prior auth form is to determine whether a specific treatment or service is medically necessary and covered under the patient's insurance plan.
What are the required documents and information for the prior auth form?
+Required documents and information include medical records, prescriptions, diagnostic reports, and a completed prior auth form.