The healthcare industry relies heavily on prior authorization forms to ensure that patients receive necessary treatments while also controlling costs. Allwell, a Medicare Advantage plan, requires healthcare providers to submit a prior authorization form for certain services or treatments. In this article, we will delve into the Allwell prior authorization form for Wellcare, its importance, and the steps involved in the process.
Understanding Prior Authorization
Prior authorization, also known as pre-authorization or pre-certification, is a process where healthcare providers must obtain approval from the patient's insurance provider before administering certain medical treatments or services. This process helps ensure that the treatment is medically necessary and meets the insurance provider's coverage guidelines.

Prior authorization is an essential step in the healthcare process, as it helps prevent unnecessary medical expenses and ensures that patients receive only the treatments they need.
The Importance of Prior Authorization
Prior authorization is crucial for several reasons:
- It helps control healthcare costs by preventing unnecessary medical expenses.
- It ensures that patients receive only the treatments they need, reducing the risk of complications or adverse reactions.
- It helps healthcare providers and insurance providers communicate effectively, ensuring that patients receive the best possible care.
Allwell Prior Authorization Form for Wellcare
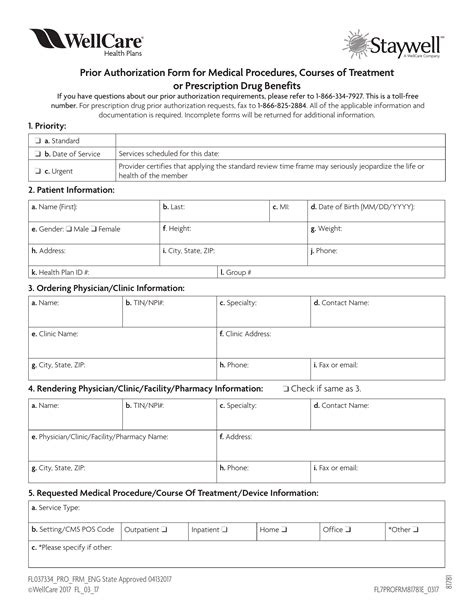
The Allwell prior authorization form for Wellcare is a document that healthcare providers must complete and submit to Allwell for review and approval. The form requires detailed information about the patient, the treatment or service being requested, and the healthcare provider's rationale for the treatment.

The form typically includes the following information:
- Patient demographics and insurance information
- Treatment or service being requested
- Healthcare provider's rationale for the treatment
- Supporting medical documentation
Steps Involved in the Prior Authorization Process
The prior authorization process involves several steps:
- Submission of the Prior Authorization Form: The healthcare provider completes and submits the prior authorization form to Allwell, along with supporting medical documentation.
- Review of the Prior Authorization Form: Allwell reviews the prior authorization form to ensure that it meets their coverage guidelines and requirements.
- Approval or Denial: Allwell approves or denies the prior authorization request, based on their review.
- Notification of the Healthcare Provider: Allwell notifies the healthcare provider of their decision, along with any additional information or requirements.
Common Reasons for Prior Authorization Denials
Prior authorization requests can be denied for several reasons, including:
- Lack of Medical Necessity: The treatment or service being requested is not medically necessary.
- Inadequate Documentation: The prior authorization form is incomplete or lacks supporting medical documentation.
- Non-Covered Service: The treatment or service being requested is not covered under the patient's insurance plan.

Appealing a Prior Authorization Denial
If a prior authorization request is denied, the healthcare provider can appeal the decision. The appeal process typically involves:
- Submission of Additional Information: The healthcare provider submits additional information or documentation to support the prior authorization request.
- Review of the Appeal: Allwell reviews the appeal and makes a decision.
- Notification of the Healthcare Provider: Allwell notifies the healthcare provider of their decision.
Conclusion
In conclusion, the Allwell prior authorization form for Wellcare is an essential document that healthcare providers must complete and submit to ensure that patients receive necessary treatments while controlling costs. Understanding the prior authorization process and the steps involved can help healthcare providers navigate the system effectively and provide the best possible care for their patients.
We hope this article has provided valuable insights into the Allwell prior authorization form for Wellcare. If you have any questions or comments, please feel free to share them below.
What is prior authorization?
+Prior authorization, also known as pre-authorization or pre-certification, is a process where healthcare providers must obtain approval from the patient's insurance provider before administering certain medical treatments or services.
Why is prior authorization important?
+Prior authorization is important because it helps control healthcare costs, ensures that patients receive only the treatments they need, and facilitates communication between healthcare providers and insurance providers.
What information is required on the Allwell prior authorization form?
+The Allwell prior authorization form requires detailed information about the patient, the treatment or service being requested, and the healthcare provider's rationale for the treatment, along with supporting medical documentation.