As a patient or healthcare provider, navigating the complexities of prior authorization requirements can be overwhelming, especially when dealing with specific medications like Stelara. Understanding the requirements for Aetna's Stelara prior authorization form is crucial to ensure timely and effective treatment.
What is Stelara?

Stelara (ustekinumab) is a prescription medication used to treat moderate to severe plaque psoriasis, psoriatic arthritis, and Crohn's disease. As a biologic medication, Stelara works by targeting specific proteins in the body that cause inflammation.
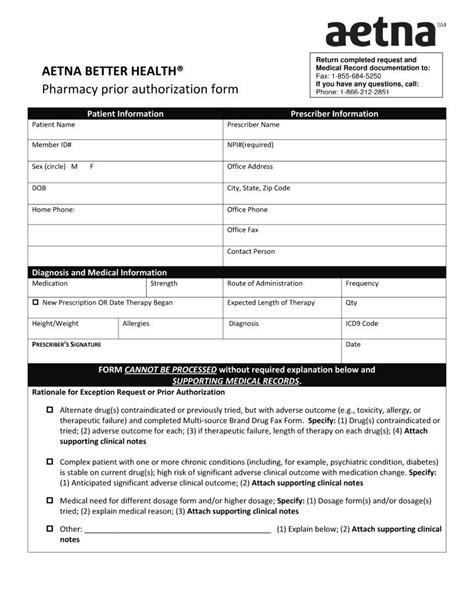
Aetna's Prior Authorization Process

Aetna requires prior authorization for Stelara to ensure that patients meet specific clinical criteria and to manage the cost of the medication. The prior authorization process typically involves submitting a request to Aetna, providing medical records and documentation to support the patient's diagnosis and treatment plan.
Required Documentation
To initiate the prior authorization process, healthcare providers must submit the following documentation:
- Patient's medical history and diagnosis
- Treatment plan, including dosage and administration instructions
- Laboratory results, including liver function tests and complete blood counts
- Records of previous treatments, including any failed or ineffective treatments
- Proof of failure or intolerance to other treatments, if applicable
Aetna Stelara Prior Authorization Form Requirements

Aetna's Stelara prior authorization form requires the following information:
- Patient demographics and contact information
- Healthcare provider information and contact details
- Diagnosis and treatment plan
- Dosage and administration instructions
- Laboratory results and medical history
- Records of previous treatments
The form must be completed in its entirety and submitted to Aetna for review. Incomplete or missing information may delay the prior authorization process.
Submission Guidelines

Completed prior authorization forms can be submitted to Aetna via:
- Fax: 1-800-414-1427
- Mail: Aetna, Prior Authorization Department, PO Box 14020, Lexington, KY 40512
- Electronic submission through Aetna's online portal
Timeline and Response

Aetna typically responds to prior authorization requests within 3-5 business days. If approved, the patient's medication will be covered, and the healthcare provider will receive notification. If denied, the patient or healthcare provider may appeal the decision.
Appeals Process

If Aetna denies a prior authorization request, patients or healthcare providers may appeal the decision. The appeals process typically involves submitting additional documentation or information to support the patient's diagnosis and treatment plan.
Conclusion
Navigating the prior authorization process for Stelara can be complex and time-consuming. Understanding Aetna's requirements and guidelines can help healthcare providers and patients ensure timely and effective treatment. By following the steps outlined above, patients can access the medication they need to manage their condition.What is the purpose of prior authorization for Stelara?
+Prior authorization is required to ensure that patients meet specific clinical criteria and to manage the cost of the medication.
What documentation is required for Stelara prior authorization?
+Required documentation includes patient demographics, medical history, treatment plan, laboratory results, and records of previous treatments.
How long does the prior authorization process typically take?
+Aetna typically responds to prior authorization requests within 3-5 business days.