Medicare prior authorization is a crucial process for healthcare providers and patients alike. It ensures that patients receive necessary medical treatments while also controlling healthcare costs. Wellcare Medicare, a prominent Medicare Advantage plan provider, requires prior authorization for certain medical services and prescriptions. In this article, we will delve into the world of Wellcare Medicare prior authorization, exploring its importance, the process, and the necessary forms.
Understanding Wellcare Medicare Prior Authorization

Prior authorization is a process where healthcare providers obtain approval from Wellcare Medicare before administering specific medical treatments or prescribing certain medications. This process helps ensure that patients receive necessary and cost-effective care. Wellcare Medicare requires prior authorization for various services, including prescription medications, medical equipment, and specialized treatments.
Why is Prior Authorization Important?
Prior authorization is essential for several reasons:
- Cost Control: By requiring prior authorization, Wellcare Medicare can control healthcare costs by ensuring that patients receive necessary and cost-effective treatments.
- Quality of Care: Prior authorization helps ensure that patients receive high-quality care by verifying the medical necessity of treatments.
- Patient Safety: Prior authorization can prevent patients from receiving unnecessary or potentially harmful treatments.
The Wellcare Medicare Prior Authorization Process

The prior authorization process for Wellcare Medicare involves the following steps:
- Determine Medical Necessity: Healthcare providers determine whether a medical treatment or prescription is medically necessary.
- Submit Prior Authorization Request: Healthcare providers submit a prior authorization request to Wellcare Medicare, providing necessary documentation and medical information.
- Review and Approval: Wellcare Medicare reviews the request and makes a determination regarding approval or denial.
- Notification: Wellcare Medicare notifies the healthcare provider and patient of the prior authorization decision.
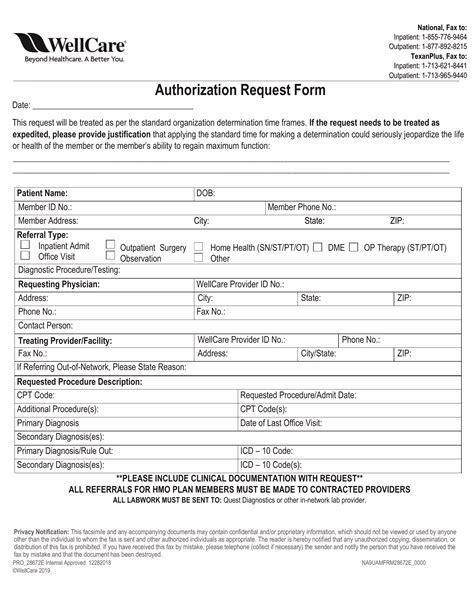
Wellcare Medicare Prior Authorization Form
The Wellcare Medicare prior authorization form is an essential document that healthcare providers must complete and submit to Wellcare Medicare. The form typically includes the following information:
- Patient Information: Patient name, date of birth, and Medicare ID number.
- Treatment Information: Description of the medical treatment or prescription, including dosage and frequency.
- Medical Necessity: Explanation of the medical necessity of the treatment or prescription.
- Supporting Documentation: Attachments of medical records, test results, and other supporting documentation.
Tips for Completing the Wellcare Medicare Prior Authorization Form

When completing the Wellcare Medicare prior authorization form, keep the following tips in mind:
- Ensure Accuracy: Verify patient information and treatment details for accuracy.
- Provide Complete Information: Include all necessary documentation and medical information to support the prior authorization request.
- Submit Timely: Submit the prior authorization request in a timely manner to avoid delays in treatment.
Common Mistakes to Avoid
When completing the Wellcare Medicare prior authorization form, avoid the following common mistakes:
- Incomplete Information: Failing to provide necessary documentation or medical information.
- Inaccurate Information: Submitting inaccurate patient information or treatment details.
- Late Submission: Submitting the prior authorization request too late, resulting in delayed treatment.
Electronic Prior Authorization for Wellcare Medicare

Wellcare Medicare offers electronic prior authorization, which allows healthcare providers to submit prior authorization requests online. This process can help reduce paperwork and speed up the approval process.
Benefits of Electronic Prior Authorization
Electronic prior authorization offers several benefits, including:
- Faster Processing: Electronic prior authorization requests are processed faster than paper-based requests.
- Reduced Paperwork: Electronic submission reduces paperwork and administrative burden.
- Increased Accuracy: Electronic submission reduces the risk of errors and inaccuracies.
Conclusion: Navigating Wellcare Medicare Prior Authorization

Navigating the Wellcare Medicare prior authorization process can be complex, but understanding the importance of prior authorization, the process, and the necessary forms can help healthcare providers and patients alike. By following the tips and avoiding common mistakes, healthcare providers can ensure that patients receive necessary medical treatments while also controlling healthcare costs.
We encourage you to share your experiences and tips for navigating the Wellcare Medicare prior authorization process in the comments below. If you have any questions or concerns, please don't hesitate to reach out.
What is Wellcare Medicare prior authorization?
+Wellcare Medicare prior authorization is a process where healthcare providers obtain approval from Wellcare Medicare before administering specific medical treatments or prescribing certain medications.
What information is required on the Wellcare Medicare prior authorization form?
+The Wellcare Medicare prior authorization form typically includes patient information, treatment information, medical necessity explanation, and supporting documentation.
Can I submit prior authorization requests electronically?
+Yes, Wellcare Medicare offers electronic prior authorization, which allows healthcare providers to submit prior authorization requests online.