The healthcare system can be complex and overwhelming, especially when it comes to dealing with insurance providers and prior authorization forms. In Illinois, BCBS (Blue Cross Blue Shield) is one of the largest health insurance providers, and navigating their prior authorization process can be a daunting task. In this article, we will break down the BCBS of Illinois prior authorization form and provide guidance on how to make the process easier.
Understanding Prior Authorization

Prior authorization is a process used by health insurance providers to determine whether a specific treatment or service is medically necessary and covered under the patient's insurance plan. This process helps ensure that patients receive necessary care while also controlling healthcare costs.
Why is Prior Authorization Necessary?
Prior authorization is necessary for several reasons:
- To ensure that patients receive medically necessary care
- To prevent unnecessary or redundant treatments
- To control healthcare costs
- To ensure that patients are receiving care that is covered under their insurance plan
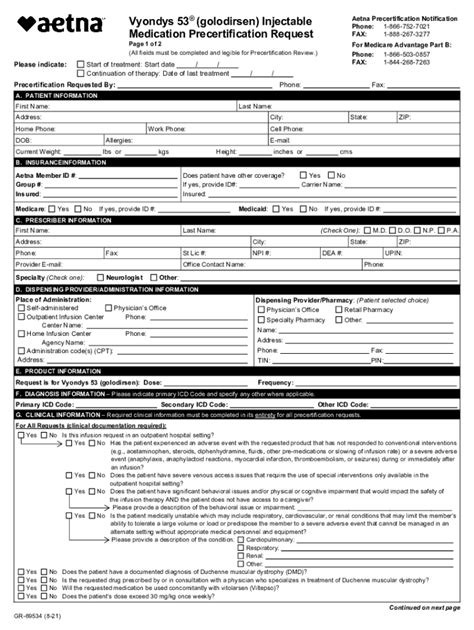
BCBS of Illinois Prior Authorization Form

The BCBS of Illinois prior authorization form is used to request approval for specific treatments or services. The form typically requires the following information:
- Patient demographics
- Treatment or service requested
- Medical necessity documentation
- Supporting clinical documentation
How to Complete the BCBS of Illinois Prior Authorization Form
To complete the BCBS of Illinois prior authorization form, follow these steps:
- Gather all necessary documentation, including patient demographics, treatment or service requested, and supporting clinical documentation.
- Complete the form accurately and thoroughly, ensuring that all required information is included.
- Submit the form to BCBS of Illinois for review and approval.
Tips for Making the Prior Authorization Process Easier

While the prior authorization process can be complex, there are several tips to make it easier:
- Understand the process: Take the time to understand the prior authorization process and what is required.
- Gather necessary documentation: Ensure that all necessary documentation is gathered and submitted with the form.
- Submit forms accurately and thoroughly: Ensure that the form is completed accurately and thoroughly to avoid delays or denials.
- Follow up: Follow up with BCBS of Illinois to ensure that the form is received and being processed.
Common Mistakes to Avoid
When completing the BCBS of Illinois prior authorization form, avoid the following common mistakes:
- Inaccurate or incomplete information: Ensure that all information is accurate and complete to avoid delays or denials.
- Missing documentation: Ensure that all necessary documentation is included with the form.
- Late submissions: Ensure that the form is submitted in a timely manner to avoid delays.
Benefits of Electronic Prior Authorization

Electronic prior authorization offers several benefits, including:
- Increased efficiency: Electronic prior authorization streamlines the process, reducing administrative burdens and increasing efficiency.
- Reduced errors: Electronic prior authorization reduces the risk of errors, ensuring that information is accurate and complete.
- Faster processing: Electronic prior authorization enables faster processing, reducing wait times for patients.
Implementing Electronic Prior Authorization
To implement electronic prior authorization, follow these steps:
- Choose an electronic prior authorization platform: Research and choose an electronic prior authorization platform that meets your needs.
- Configure the platform: Configure the platform to meet your specific needs and requirements.
- Train staff: Train staff on the use of the platform to ensure a smooth transition.
Conclusion
The BCBS of Illinois prior authorization form can be complex and overwhelming, but by understanding the process and following the tips outlined in this article, you can make the process easier. Electronic prior authorization offers several benefits, including increased efficiency, reduced errors, and faster processing. By implementing electronic prior authorization, you can streamline the process and improve patient care.We would love to hear from you! Share your experiences with the BCBS of Illinois prior authorization form and any tips you have for making the process easier.
What is prior authorization?
+Prior authorization is a process used by health insurance providers to determine whether a specific treatment or service is medically necessary and covered under the patient's insurance plan.
Why is prior authorization necessary?
+Prior authorization is necessary to ensure that patients receive medically necessary care, prevent unnecessary or redundant treatments, control healthcare costs, and ensure that patients are receiving care that is covered under their insurance plan.
What is the BCBS of Illinois prior authorization form?
+The BCBS of Illinois prior authorization form is used to request approval for specific treatments or services. The form typically requires patient demographics, treatment or service requested, medical necessity documentation, and supporting clinical documentation.