The healthcare industry has witnessed a significant transformation in recent years, with a growing emphasis on cost containment and improved patient outcomes. One crucial aspect of this transformation is the prior authorization process, which enables healthcare providers to obtain pre-approval for specific treatments, medications, or services from insurance companies or payers. In this context, the Valenz prior authorization form has emerged as a vital tool, facilitating the exchange of information between healthcare providers, payers, and patients. In this article, we will delve into the world of prior authorization, exploring the Valenz prior authorization form, its requirements, and its significance in the healthcare ecosystem.
Understanding Prior Authorization

Prior authorization, also known as pre-certification or pre-authorization, is a process that requires healthcare providers to obtain approval from payers before administering specific treatments, medications, or services to patients. This process is designed to ensure that patients receive necessary and evidence-based care while controlling healthcare costs. Prior authorization is commonly required for specialized treatments, expensive medications, or services that are not deemed medically necessary.
Benefits of Prior Authorization
Prior authorization offers several benefits to patients, healthcare providers, and payers:
- Ensures that patients receive necessary and evidence-based care
- Helps control healthcare costs by reducing unnecessary treatments and services
- Facilitates communication between healthcare providers, payers, and patients
- Streamlines the care delivery process
Valenz Prior Authorization Form: An Overview

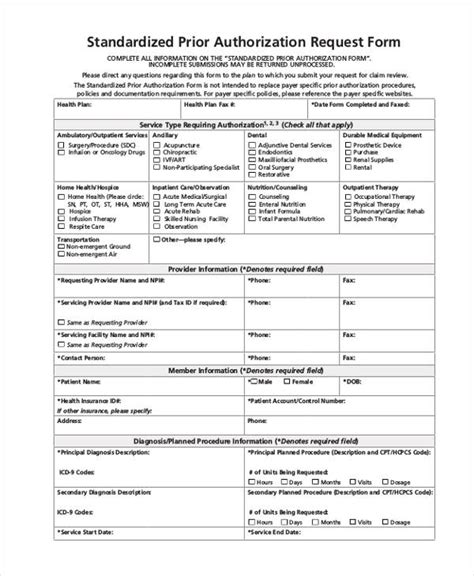
The Valenz prior authorization form is a standardized document used by healthcare providers to request prior authorization from payers. This form typically includes essential information about the patient, the requested treatment or service, and the healthcare provider. The Valenz prior authorization form is designed to simplify the prior authorization process, reducing administrative burdens and facilitating communication between stakeholders.
Key Components of the Valenz Prior Authorization Form
The Valenz prior authorization form typically includes the following key components:
- Patient information: name, date of birth, insurance details, and medical history
- Healthcare provider information: name, contact details, and qualifications
- Requested treatment or service: description, diagnosis, and treatment plan
- Supporting documentation: medical records, test results, and clinical notes
Requirements for Completing the Valenz Prior Authorization Form

To complete the Valenz prior authorization form, healthcare providers must ensure that they have the following information and documentation:
- Accurate patient information and medical history
- Clear description of the requested treatment or service
- Supporting documentation, such as medical records and test results
- Healthcare provider qualifications and contact details
- Compliance with payer-specific requirements and guidelines
Common Challenges and Solutions
Healthcare providers may encounter several challenges when completing the Valenz prior authorization form, including:
- Incomplete or inaccurate patient information
- Insufficient supporting documentation
- Difficulty navigating payer-specific requirements and guidelines
To overcome these challenges, healthcare providers can:
- Verify patient information and medical history before submitting the form
- Ensure that supporting documentation is complete and accurate
- Familiarize themselves with payer-specific requirements and guidelines
- Utilize electronic prior authorization platforms to streamline the process
Streamlining the Prior Authorization Process

The prior authorization process can be time-consuming and administrative-intensive, requiring significant resources and effort from healthcare providers. To streamline this process, healthcare providers can:
- Utilize electronic prior authorization platforms
- Implement automated workflows and notifications
- Develop relationships with payers and their representatives
- Educate patients about the prior authorization process and its benefits
Best Practices for Prior Authorization
To ensure a smooth and efficient prior authorization process, healthcare providers can follow these best practices:
- Verify patient information and medical history before submitting the form
- Ensure that supporting documentation is complete and accurate
- Familiarize themselves with payer-specific requirements and guidelines
- Utilize electronic prior authorization platforms to streamline the process
By following these best practices and utilizing the Valenz prior authorization form, healthcare providers can simplify the prior authorization process, reduce administrative burdens, and improve patient outcomes.
What is prior authorization?
+Prior authorization, also known as pre-certification or pre-authorization, is a process that requires healthcare providers to obtain approval from payers before administering specific treatments, medications, or services to patients.
What is the Valenz prior authorization form?
+The Valenz prior authorization form is a standardized document used by healthcare providers to request prior authorization from payers. This form typically includes essential information about the patient, the requested treatment or service, and the healthcare provider.
What are the benefits of prior authorization?
+Prior authorization offers several benefits to patients, healthcare providers, and payers, including ensuring that patients receive necessary and evidence-based care, controlling healthcare costs, and facilitating communication between stakeholders.
In conclusion, the Valenz prior authorization form is a vital tool in the healthcare ecosystem, facilitating the exchange of information between healthcare providers, payers, and patients. By understanding the prior authorization process, the requirements of the Valenz prior authorization form, and the benefits of prior authorization, healthcare providers can simplify the prior authorization process, reduce administrative burdens, and improve patient outcomes. We encourage you to share your thoughts and experiences with prior authorization in the comments below.