As a healthcare provider, you understand the importance of ensuring that your patients receive the medications they need to manage their conditions effectively. However, with the increasing complexity of healthcare regulations and insurance requirements, obtaining prior authorization for certain medications can be a daunting task. In this article, we will focus on the Silverscript prior authorization form, providing a step-by-step guide to help you navigate the process with ease.
The Importance of Prior Authorization
Prior authorization is a process that requires healthcare providers to obtain approval from a patient's insurance provider before prescribing certain medications or treatments. This process is designed to ensure that patients receive safe and effective treatments while also controlling healthcare costs. Silverscript, a popular Medicare Part D prescription drug plan, requires prior authorization for certain medications to ensure that patients receive the most cost-effective and clinically appropriate treatments.
Understanding the Silverscript Prior Authorization Form
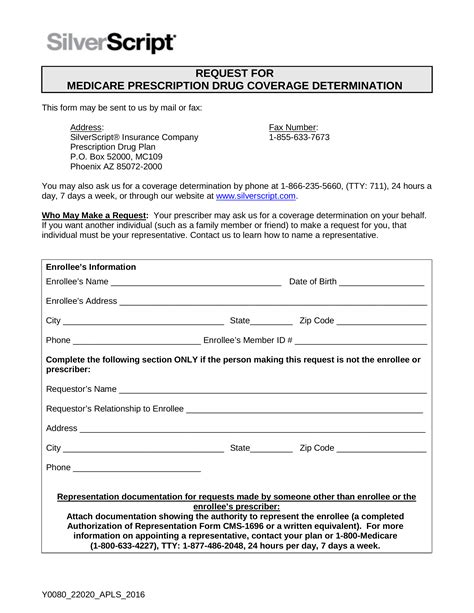
The Silverscript prior authorization form is a standardized document that healthcare providers must complete and submit to Silverscript for review. The form requires providers to provide detailed information about the patient's medical condition, the prescribed medication, and the rationale for the treatment. To ensure a smooth prior authorization process, it is essential to understand the form's requirements and submit accurate and complete information.
Step-by-Step Guide to Completing the Silverscript Prior Authorization Form

Step 1: Gather Patient Information
Before starting the prior authorization process, gather the patient's relevant medical information, including:
- Patient demographics (name, date of birth, etc.)
- Medical history and current diagnosis
- Medication list (including dosages and frequencies)
- Laboratory results and other relevant test results
Step 2: Determine the Type of Prior Authorization
Silverscript requires prior authorization for certain medications, including:
- Non-formulary medications
- Quantity limits
- Step therapy
- Prior authorization for specific medical conditions (e.g., cancer, HIV/AIDS)
Determine the type of prior authorization required for the patient's medication and ensure that you have the necessary documentation to support the request.
Step 3: Complete the Prior Authorization Form
Complete the Silverscript prior authorization form, providing accurate and detailed information about the patient's medical condition, the prescribed medication, and the rationale for the treatment. The form typically requires the following information:
- Patient demographics
- Medical history and current diagnosis
- Medication information (including dosages and frequencies)
- Rationale for the treatment
- Supporting documentation (e.g., laboratory results, medical records)
Step 4: Submit the Prior Authorization Request
Submit the completed prior authorization form to Silverscript via fax, mail, or electronically through their online portal. Ensure that you include all required documentation and information to avoid delays or denials.
Step 5: Follow-up on the Prior Authorization Request
After submitting the prior authorization request, follow up with Silverscript to ensure that the request is being processed. You can check the status of the request online or by contacting Silverscript's customer service department.
Common Mistakes to Avoid When Completing the Silverscript Prior Authorization Form

- Incomplete or inaccurate information
- Missing or incomplete supporting documentation
- Failure to submit the request in a timely manner
- Failure to follow up on the request
Benefits of Using the Silverscript Prior Authorization Form

- Streamlined prior authorization process
- Reduced administrative burden
- Improved patient outcomes
- Enhanced provider-patient communication
Conclusion: Navigating the Silverscript Prior Authorization Process with Ease
Navigating the Silverscript prior authorization process can be complex, but by following the step-by-step guide outlined above, healthcare providers can ensure a smooth and efficient process. Remember to gather accurate and complete information, determine the type of prior authorization required, complete the form carefully, submit the request in a timely manner, and follow up on the request. By avoiding common mistakes and leveraging the benefits of the Silverscript prior authorization form, providers can improve patient outcomes and enhance the overall quality of care.
We invite you to share your experiences and tips for navigating the Silverscript prior authorization process in the comments below. Your feedback is invaluable in helping us improve our content and provide the most accurate and helpful information for healthcare providers.
What is the purpose of the Silverscript prior authorization form?
+The Silverscript prior authorization form is designed to ensure that patients receive safe and effective treatments while controlling healthcare costs.
What type of information is required on the Silverscript prior authorization form?
+The form requires accurate and detailed information about the patient's medical condition, the prescribed medication, and the rationale for the treatment.
How do I submit the Silverscript prior authorization form?
+The form can be submitted via fax, mail, or electronically through Silverscript's online portal.