Receiving medical care can be a daunting experience, especially when dealing with the complexities of insurance coverage. Tricare, a healthcare program for military personnel and their families, has its own set of requirements for prior authorization. This process can seem overwhelming, but understanding the steps to complete the Tricare prior authorization form can make a significant difference in ensuring timely and effective care.
Understanding Tricare Prior Authorization

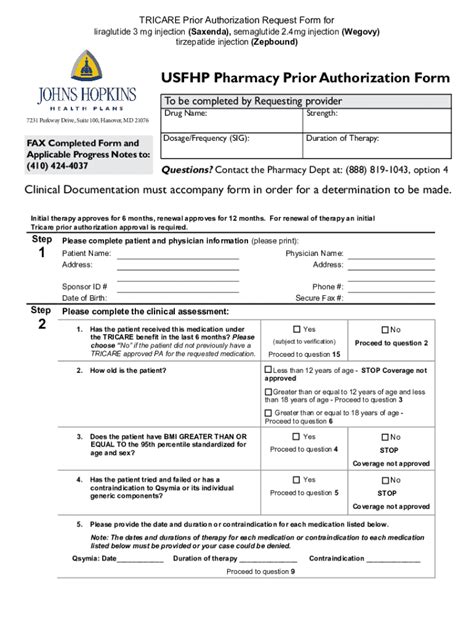
Prior authorization is a process that requires healthcare providers to obtain approval from Tricare before rendering certain medical services. This ensures that patients receive necessary care while also controlling healthcare costs. The Tricare prior authorization form is a crucial document that must be completed accurately to avoid delays or denials of coverage.
Method 1: Completing the Form Online

One of the most convenient ways to complete the Tricare prior authorization form is online. Tricare's website provides a secure portal for healthcare providers to submit the necessary information. To complete the form online, providers will need to:
- Log in to the Tricare website using their credentials
- Select the "Prior Authorization" option
- Fill out the required fields, including patient information, medical history, and treatment details
- Upload supporting documentation, if necessary
- Submit the form for review
Benefits of Online Submission
- Faster processing times
- Reduced paperwork and administrative burdens
- Increased accuracy and reduced errors
Method 2: Faxing the Completed Form

For providers who prefer a more traditional approach, faxing the completed Tricare prior authorization form is a viable option. To fax the form, providers will need to:
- Complete the form accurately and thoroughly
- Ensure all required documentation is included
- Fax the form to the designated Tricare fax number
- Verify receipt of the faxed form with Tricare
Important Considerations
- Ensure the fax number is correct to avoid delays
- Confirm receipt of the faxed form to avoid lost or misplaced documents
Method 3: Mailing the Completed Form

Mailing the completed Tricare prior authorization form is another option for providers. To mail the form, providers will need to:
- Complete the form accurately and thoroughly
- Ensure all required documentation is included
- Mail the form to the designated Tricare address
- Verify receipt of the mailed form with Tricare
Important Considerations
- Ensure the address is correct to avoid delays
- Use certified mail or tracking to confirm receipt of the mailed form
Method 4: Using a Third-Party Prior Authorization Service

For providers who prefer to outsource prior authorization tasks, third-party services are available. These services specialize in navigating the complexities of prior authorization and can help streamline the process. To use a third-party service, providers will need to:
- Research and select a reputable prior authorization service
- Provide the necessary information and documentation
- Allow the third-party service to handle the prior authorization process
Benefits of Third-Party Services
- Reduced administrative burdens
- Increased efficiency and accuracy
- Expertise in navigating prior authorization complexities
Method 5: Working with a Medical Billing Service

Medical billing services specialize in handling the business side of healthcare, including prior authorization. These services can help providers navigate the Tricare prior authorization process and ensure accurate and timely submissions. To work with a medical billing service, providers will need to:
- Research and select a reputable medical billing service
- Provide the necessary information and documentation
- Allow the medical billing service to handle the prior authorization process
Benefits of Medical Billing Services
- Reduced administrative burdens
- Increased efficiency and accuracy
- Expertise in navigating medical billing complexities
What is the purpose of Tricare prior authorization?
+Tricare prior authorization is a process that requires healthcare providers to obtain approval from Tricare before rendering certain medical services. This ensures that patients receive necessary care while also controlling healthcare costs.
How do I submit a Tricare prior authorization form?
+Tricare prior authorization forms can be submitted online, by fax, or by mail. Providers can also use third-party prior authorization services or work with a medical billing service to handle the process.
What information is required on the Tricare prior authorization form?
+The Tricare prior authorization form requires patient information, medical history, treatment details, and supporting documentation. Providers must ensure all required fields are completed accurately and thoroughly.
By understanding the different methods for completing the Tricare prior authorization form, healthcare providers can ensure accurate and timely submissions. This, in turn, helps patients receive the necessary care without delays or denials of coverage. Whether submitting online, by fax, or by mail, or working with a third-party service, providers can navigate the complexities of Tricare prior authorization with confidence.