The world of healthcare can be complex and overwhelming, especially when it comes to navigating the process of prior authorization. For patients and healthcare providers in Tennessee, understanding the TennCare prior authorization form is crucial to ensure seamless access to necessary medical treatments. In this article, we will delve into the intricacies of the TennCare prior authorization form, providing a step-by-step guide to help you navigate this process with ease.

What is TennCare Prior Authorization?
TennCare is Tennessee's Medicaid program, providing healthcare coverage to low-income individuals and families. Prior authorization is a process that requires healthcare providers to obtain approval from TennCare before administering certain medical treatments or services. This process aims to ensure that patients receive necessary and cost-effective care while minimizing unnecessary expenses.
Why is Prior Authorization Necessary?
Prior authorization is essential to ensure that patients receive the right treatment at the right time. It helps to:
- Verify the medical necessity of a treatment or service
- Ensure that the treatment is covered under the patient's insurance plan
- Prevent unnecessary costs and reduce healthcare expenses
- Promote the use of evidence-based treatments and guidelines
Step 1: Understanding the Prior Authorization Process
The prior authorization process typically involves the following steps:
- Patient Referral: A healthcare provider refers a patient for a specific treatment or service.
- Prior Authorization Request: The healthcare provider submits a prior authorization request to TennCare, including the patient's medical history, treatment plan, and other relevant information.
- TennCare Review: TennCare reviews the prior authorization request to determine whether the treatment is medically necessary and covered under the patient's insurance plan.
- Approval or Denial: TennCare issues a decision, either approving or denying the prior authorization request.

Step 2: Gathering Required Information
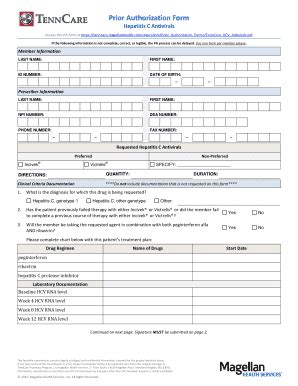
To complete the prior authorization form, healthcare providers will need to gather the following information:
- Patient Information: Patient name, date of birth, and TennCare ID number
- Treatment Information: Description of the treatment or service, including the type, frequency, and duration
- Medical History: Patient's medical history, including relevant diagnoses, test results, and treatment outcomes
- Supporting Documentation: Supporting documentation, such as medical records, test results, and treatment plans
Tips for Gathering Required Information
- Ensure that all patient information is accurate and up-to-date
- Clearly describe the treatment or service, including any relevant details
- Include all relevant medical history and supporting documentation
Step 3: Completing the Prior Authorization Form
The prior authorization form can be completed online or by fax. Healthcare providers should ensure that all required information is included and that the form is completed accurately and thoroughly.

Tips for Completing the Prior Authorization Form
- Ensure that all required fields are completed accurately and thoroughly
- Include all relevant supporting documentation
- Review the form carefully before submitting it
Step 4: Submitting the Prior Authorization Form
The completed prior authorization form can be submitted online or by fax. Healthcare providers should ensure that the form is submitted in a timely manner to avoid delays in the approval process.
Tips for Submitting the Prior Authorization Form
- Submit the form as soon as possible to avoid delays
- Ensure that the form is complete and accurate before submitting it
- Keep a record of the submission, including the date and time
Step 5: Following Up on the Prior Authorization Request
Healthcare providers should follow up on the prior authorization request to ensure that it is being processed in a timely manner.

Tips for Following Up on the Prior Authorization Request
- Follow up on the request within 3-5 business days
- Ensure that the request is being processed and that a decision is pending
- Keep a record of all follow-up attempts
Conclusion
Navigating the TennCare prior authorization form can be complex, but by following these steps, healthcare providers can ensure that their patients receive the necessary medical treatments and services. By understanding the prior authorization process, gathering required information, completing the prior authorization form, submitting the form, and following up on the request, healthcare providers can help their patients access the care they need.

We encourage you to share your experiences and tips for navigating the TennCare prior authorization form in the comments below. By working together, we can ensure that patients receive the care they need and deserve.
What is the purpose of the TennCare prior authorization form?
+The TennCare prior authorization form is used to request approval for certain medical treatments or services. It helps to ensure that patients receive necessary and cost-effective care while minimizing unnecessary expenses.
How long does the prior authorization process typically take?
+The prior authorization process typically takes 3-5 business days. However, this timeframe may vary depending on the complexity of the request and the availability of necessary information.
What information is required to complete the prior authorization form?
+The prior authorization form requires patient information, treatment information, medical history, and supporting documentation. Healthcare providers should ensure that all required information is included and that the form is completed accurately and thoroughly.