Streamlining the Prior Authorization Process with Silver Script

Prior authorization is an essential step in ensuring that patients receive the necessary medication and treatments while controlling healthcare costs. However, the process can be lengthy and bureaucratic, leading to delays and frustration for patients, healthcare providers, and pharmacists. Silver Script, a leading pharmacy benefit management company, has introduced a simplified prior authorization process to alleviate these concerns.
In this article, we will guide you through the 5 easy steps to complete a Silver Script prior auth form, making it easier for healthcare providers to navigate the process and get their patients the treatments they need.
The Importance of Prior Authorization
Prior authorization is a critical step in the healthcare process that ensures patients receive the necessary medication and treatments while controlling healthcare costs. It involves verifying that a prescribed treatment or medication is medically necessary and meets specific criteria before it is approved. This process helps prevent unnecessary treatments, reduces healthcare costs, and ensures that patients receive the most effective care.
Step 1: Gather Required Information

The first step in completing a Silver Script prior auth form is to gather all the required information. This includes:
- Patient demographics (name, date of birth, address, etc.)
- Prescribed medication or treatment details (name, dosage, frequency, etc.)
- Medical condition or diagnosis
- Relevant medical history
- Current medications and dosages
Having all the necessary information readily available will make the process smoother and reduce the likelihood of errors or delays.
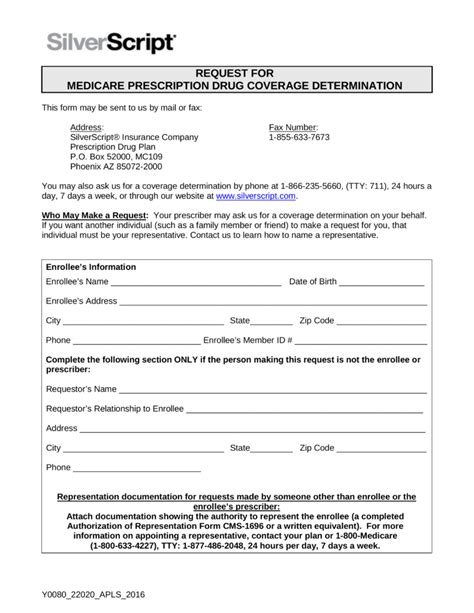
Step 2: Choose the Correct Prior Auth Form
Silver Script provides different prior auth forms for various medications and treatments. It is essential to choose the correct form to ensure that the request is processed efficiently. You can find the correct form on the Silver Script website or by contacting their customer service.
Step 3: Complete the Prior Auth Form

Once you have gathered all the required information and chosen the correct form, complete the prior auth form carefully. Make sure to:
- Fill out all the required fields accurately
- Attach supporting documentation (e.g., medical records, test results)
- Sign and date the form
Incomplete or inaccurate forms may lead to delays or rejection, so it is crucial to double-check the information before submitting.
Step 4: Submit the Prior Auth Form
After completing the prior auth form, submit it to Silver Script for review. You can fax, email, or mail the form, depending on your preference. Make sure to follow the submission guidelines provided by Silver Script to ensure timely processing.
Step 5: Follow Up on the Prior Auth Request

Once you have submitted the prior auth form, follow up on the request to ensure it is being processed. You can check the status of the request online or contact Silver Script's customer service for updates.
By following these 5 easy steps, healthcare providers can simplify the prior authorization process and ensure that their patients receive the necessary treatments in a timely manner.
Benefits of Streamlining the Prior Authorization Process
Streamlining the prior authorization process with Silver Script offers several benefits, including:
- Reduced administrative burden for healthcare providers
- Faster processing times for prior auth requests
- Improved patient outcomes due to timely access to necessary treatments
- Enhanced patient satisfaction
- Cost savings for patients and healthcare providers
By implementing a simplified prior authorization process, Silver Script aims to alleviate the administrative burden on healthcare providers, allowing them to focus on providing quality patient care.
Conclusion
Completing a Silver Script prior auth form is a straightforward process that can be done in 5 easy steps. By gathering required information, choosing the correct form, completing the form accurately, submitting it for review, and following up on the request, healthcare providers can ensure that their patients receive the necessary treatments in a timely manner. Streamlining the prior authorization process with Silver Script offers numerous benefits, including reduced administrative burden, faster processing times, and improved patient outcomes.
What is prior authorization, and why is it necessary?
+Prior authorization is a process that verifies that a prescribed treatment or medication is medically necessary and meets specific criteria before it is approved. It helps prevent unnecessary treatments, reduces healthcare costs, and ensures that patients receive the most effective care.
How long does the prior authorization process take?
+The prior authorization process can take anywhere from a few days to several weeks, depending on the complexity of the request and the speed of the healthcare provider's submission.
What happens if the prior auth request is denied?
+If the prior auth request is denied, the healthcare provider can appeal the decision by providing additional information or supporting documentation. The patient may also be able to request a review of the decision.