Prior authorization forms are a crucial part of the healthcare system, ensuring that patients receive the necessary care while minimizing unnecessary costs. However, for healthcare providers, filling out these forms can be a time-consuming and tedious process. The Uniform Prior Authorization Form (UPHP) is designed to streamline this process, but it can still be overwhelming. In this article, we will discuss five ways to simplify the UPHP prior authorization form, making it easier for healthcare providers to focus on what matters most – patient care.
Understanding the UPHP Prior Authorization Form

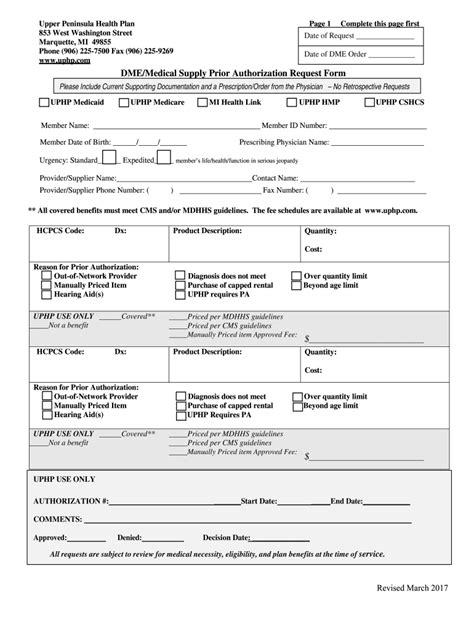
The UPHP prior authorization form is a standardized document used by healthcare providers to request approval for certain treatments, medications, or services. The form requires detailed information about the patient's condition, treatment plan, and medical history. While the form is designed to be comprehensive, it can be lengthy and complex, leading to frustration and delays.
1. Implement Electronic Prior Authorization (ePA)

One way to simplify the UPHP prior authorization form is to implement electronic prior authorization (ePA). ePA allows healthcare providers to submit prior authorization requests electronically, reducing paperwork and administrative burdens. This not only saves time but also minimizes errors and improves the overall efficiency of the prior authorization process.
Benefits of ePA
• Faster turnaround times • Reduced paperwork and administrative costs • Improved accuracy and reduced errors • Enhanced patient satisfaction
2. Use Prior Authorization Software

Prior authorization software can also simplify the UPHP prior authorization form process. This software automates the prior authorization workflow, allowing healthcare providers to easily manage and track prior authorization requests. With prior authorization software, providers can:
Key Features of Prior Authorization Software
• Automate prior authorization workflows • Track and manage prior authorization requests • Integrate with electronic health records (EHRs) • Analyze prior authorization data and trends
3. Simplify the UPHP Form itself

Another way to simplify the UPHP prior authorization form is to revise the form itself. By removing unnecessary fields and making the form more concise, healthcare providers can save time and reduce administrative burdens. A simplified UPHP form can also reduce errors and improve the overall quality of prior authorization requests.
Best Practices for Simplifying the UPHP Form
• Remove unnecessary fields and sections • Use clear and concise language • Use electronic signatures and online submissions • Provide clear instructions and guidelines
4. Improve Communication and Collaboration

Effective communication and collaboration between healthcare providers, payers, and patients are critical to simplifying the UPHP prior authorization form process. By improving communication and collaboration, healthcare providers can:
Benefits of Improved Communication and Collaboration
• Reduce prior authorization denials and appeals • Improve patient satisfaction and outcomes • Enhance provider-payer relationships • Streamline the prior authorization process
5. Leverage Artificial Intelligence (AI) and Machine Learning (ML)

Finally, leveraging artificial intelligence (AI) and machine learning (ML) can simplify the UPHP prior authorization form process. AI and ML can automate prior authorization workflows, analyze prior authorization data, and provide insights and recommendations to healthcare providers.
Benefits of AI and ML in Prior Authorization
• Automate prior authorization workflows • Analyze prior authorization data and trends • Provide insights and recommendations • Improve patient outcomes and satisfaction
By implementing these five strategies, healthcare providers can simplify the UPHP prior authorization form process, reducing administrative burdens and improving patient care. Whether through electronic prior authorization, prior authorization software, or leveraging AI and ML, there are many ways to streamline the prior authorization process and improve healthcare outcomes.
We hope this article has provided valuable insights and suggestions for simplifying the UPHP prior authorization form. Share your thoughts and experiences in the comments below!
What is the UPHP prior authorization form?
+The UPHP prior authorization form is a standardized document used by healthcare providers to request approval for certain treatments, medications, or services.
How can I simplify the UPHP prior authorization form process?
+There are several ways to simplify the UPHP prior authorization form process, including implementing electronic prior authorization, using prior authorization software, simplifying the UPHP form itself, improving communication and collaboration, and leveraging AI and ML.
What are the benefits of electronic prior authorization?
+The benefits of electronic prior authorization include faster turnaround times, reduced paperwork and administrative costs, improved accuracy and reduced errors, and enhanced patient satisfaction.