OptumRx is a leading pharmacy benefit management organization that provides a range of services to help manage prescription drug benefits. One of the key services offered by OptumRx is prior authorization, which is a process that requires healthcare providers to obtain approval from the insurance company before prescribing certain medications. In this article, we will focus on the OptumRx Ozempic prior authorization form and provide a step-by-step guide on how to complete it.

Understanding the Importance of Prior Authorization
Prior authorization is an essential process in the healthcare industry, as it helps ensure that patients receive safe and effective treatment while also controlling healthcare costs. By requiring prior authorization for certain medications, insurance companies like OptumRx can verify that the prescribed treatment is medically necessary and aligns with the patient's specific needs.
Ozempic is a medication used to treat type 2 diabetes, and it is one of the medications that require prior authorization from OptumRx. The prior authorization process for Ozempic involves submitting a form to OptumRx, which will be reviewed to determine whether the medication is approved for coverage.
Benefits of Prior Authorization
While the prior authorization process may seem tedious, it has several benefits for patients, healthcare providers, and insurance companies. Some of the benefits include:
- Ensures that patients receive safe and effective treatment
- Helps control healthcare costs by reducing unnecessary prescriptions
- Allows insurance companies to verify the medical necessity of prescribed treatments
- Enables healthcare providers to prescribe medications that are aligned with the patient's specific needs
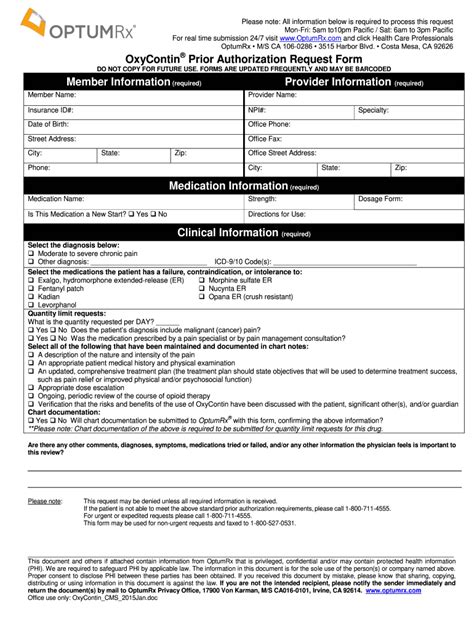
Step-by-Step Guide to Completing the OptumRx Ozempic Prior Authorization Form
Completing the OptumRx Ozempic prior authorization form requires careful attention to detail and accurate information. Here is a step-by-step guide to help you complete the form:

Step 1: Download and Print the Form
The first step is to download and print the OptumRx Ozempic prior authorization form from the OptumRx website. You can also obtain the form from your healthcare provider or by contacting OptumRx directly.
Step 2: Complete the Patient Information Section
The patient information section requires you to provide demographic information about the patient, including their name, date of birth, and contact information. Make sure to complete this section accurately and thoroughly.
Step 3: Complete the Medication Information Section
The medication information section requires you to provide information about the prescribed medication, including the name, strength, and dosage. You will also need to provide information about the patient's medical condition and the reason for prescribing Ozempic.
Step 4: Complete the Healthcare Provider Information Section
The healthcare provider information section requires you to provide information about the healthcare provider, including their name, contact information, and license number. Make sure to complete this section accurately and thoroughly.
Step 5: Sign and Date the Form
Once you have completed all the necessary sections, sign and date the form. This is an important step, as it verifies that the information provided is accurate and complete.
Common Mistakes to Avoid When Completing the Form
When completing the OptumRx Ozempic prior authorization form, there are several common mistakes to avoid. These include:
- Incomplete or inaccurate information
- Failure to sign and date the form
- Not providing sufficient medical justification for the prescribed treatment
- Not including all required documentation

What to Expect After Submitting the Form
After submitting the OptumRx Ozempic prior authorization form, you can expect a response from OptumRx within a few days. The response will indicate whether the medication has been approved for coverage or if additional information is required.
Conclusion and Next Steps
Completing the OptumRx Ozempic prior authorization form requires careful attention to detail and accurate information. By following the step-by-step guide outlined in this article, you can ensure that the form is completed correctly and efficiently. If you have any questions or concerns about the prior authorization process, don't hesitate to contact OptumRx or your healthcare provider.

We hope this article has been informative and helpful. If you have any questions or comments, please feel free to share them below.
What is the purpose of the OptumRx Ozempic prior authorization form?
+The purpose of the OptumRx Ozempic prior authorization form is to verify that the prescribed medication is medically necessary and aligns with the patient's specific needs.
How long does it take to complete the OptumRx Ozempic prior authorization form?
+The time it takes to complete the form may vary depending on the complexity of the case and the accuracy of the information provided. On average, it may take around 10-15 minutes to complete the form.
What happens if the medication is not approved for coverage?
+If the medication is not approved for coverage, the patient may need to try alternative treatments or appeal the decision. The healthcare provider can work with OptumRx to determine the best course of action.