Molina Medicaid has become a crucial healthcare provider for millions of Americans, offering a range of medical services and insurance plans to low-income individuals and families. One of the essential steps in accessing these services is completing the prior authorization form, a process that can sometimes seem daunting. In this article, we will break down the Molina Medicaid prior authorization form, explaining its purpose, requirements, and steps to complete it successfully.
The prior authorization process is a critical component of healthcare management, ensuring that patients receive the necessary treatments and medications while controlling costs and ensuring the most effective care. For healthcare providers and patients alike, understanding the prior authorization process is vital to navigating the Molina Medicaid system efficiently.

What is Prior Authorization in Molina Medicaid?
Prior authorization, also known as pre-authorization or pre-certification, is a process used by Molina Medicaid to determine whether a particular treatment, service, or medication is medically necessary and covered under the patient's insurance plan. This process involves reviewing the patient's medical information and the requested service to ensure that it meets Molina Medicaid's coverage criteria.
Why is Prior Authorization Necessary?
Prior authorization is necessary for several reasons:
- Ensures that patients receive medically necessary treatments and medications.
- Helps control healthcare costs by preventing unnecessary or duplicate services.
- Promotes effective care by encouraging the use of evidence-based treatments and medications.
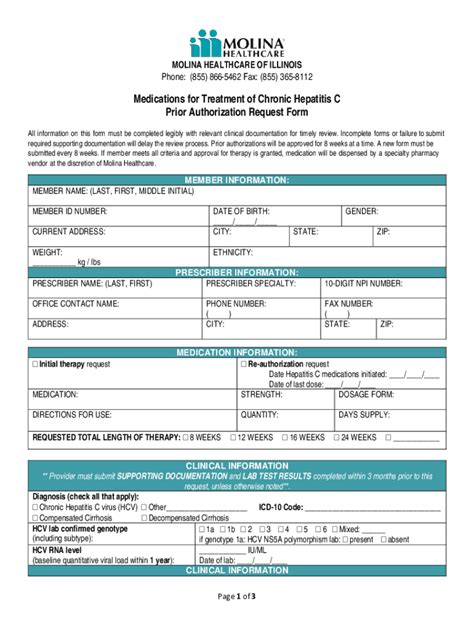
How to Complete the Molina Medicaid Prior Authorization Form
Completing the prior authorization form requires careful attention to detail and timely submission. Here are the steps to follow:
- Determine if Prior Authorization is Required: Check Molina Medicaid's website or contact their customer service to determine if prior authorization is required for the specific service or medication.
- Gather Required Information: Collect the patient's medical records, including diagnosis, treatment plans, and relevant test results.
- Complete the Prior Authorization Form: Fill out the prior authorization form, ensuring that all required fields are completed accurately and thoroughly.
- Submit the Form: Submit the completed form to Molina Medicaid via fax, mail, or online portal, depending on the preferred method.

What Information is Required on the Prior Authorization Form?
The prior authorization form typically requires the following information:
- Patient demographics, including name, date of birth, and Medicaid ID number.
- Medical information, including diagnosis, treatment plans, and relevant test results.
- Service or medication information, including the type of service or medication requested and the frequency of treatment.
Tips for a Successful Prior Authorization
To ensure a successful prior authorization, follow these tips:
- Submit Complete and Accurate Information: Ensure that all required fields are completed accurately and thoroughly.
- Submit the Form Timely: Submit the completed form to Molina Medicaid in a timely manner to avoid delays in treatment.
- Follow Up: Follow up with Molina Medicaid to ensure that the prior authorization is processed and approved.

Common Challenges and Solutions
Common challenges and solutions:
- Incomplete or Inaccurate Information: Ensure that all required fields are completed accurately and thoroughly.
- Delayed Submission: Submit the completed form to Molina Medicaid in a timely manner to avoid delays in treatment.
What to Expect After Submitting the Prior Authorization Form
After submitting the prior authorization form, you can expect:
- Processing and Review: Molina Medicaid will review the prior authorization form and medical information to determine whether the requested service or medication is medically necessary and covered under the patient's insurance plan.
- Approval or Denial: Molina Medicaid will notify the healthcare provider and patient of the prior authorization decision, either approving or denying the requested service or medication.

Conclusion
In conclusion, completing the Molina Medicaid prior authorization form is a critical step in accessing necessary medical services and medications. By understanding the prior authorization process, requirements, and steps to complete the form, healthcare providers and patients can navigate the Molina Medicaid system efficiently. Remember to submit complete and accurate information, follow up on the status of the prior authorization, and be prepared for the outcome.
We invite you to share your experiences with the Molina Medicaid prior authorization process in the comments below. Your feedback is valuable to us, and we appreciate your input.
What is the purpose of prior authorization in Molina Medicaid?
+The purpose of prior authorization is to determine whether a particular treatment, service, or medication is medically necessary and covered under the patient's insurance plan.
How do I know if prior authorization is required for a specific service or medication?
+Check Molina Medicaid's website or contact their customer service to determine if prior authorization is required for the specific service or medication.
What information is required on the prior authorization form?
+The prior authorization form typically requires patient demographics, medical information, and service or medication information.