MetroPlus is a health insurance plan that provides affordable coverage to eligible New Yorkers. Like many health insurance providers, MetroPlus requires prior authorization for certain medical procedures and medications to ensure that their members receive necessary and cost-effective care. The MetroPlus prior authorization form is a crucial document that healthcare providers must submit to obtain approval for these services. In this article, we will guide you through the process of completing the MetroPlus prior authorization form, highlighting the key sections, requirements, and tips for a successful submission.
Understanding Prior Authorization
Prior authorization is a process used by health insurance providers to review the medical necessity of certain treatments, procedures, and medications before they are administered or prescribed. This process helps to ensure that patients receive necessary care while minimizing unnecessary costs. MetroPlus requires prior authorization for various services, including hospital stays, surgical procedures, durable medical equipment, and certain medications.

Gathering Required Information
Before starting the prior authorization process, healthcare providers must gather all necessary information and documents. This includes:
- Patient's demographic information (name, date of birth, address, etc.)
- Patient's MetroPlus ID number
- Diagnosis and medical condition requiring treatment
- Treatment plan and proposed services
- Medication list and dosages
- Relevant medical records and test results
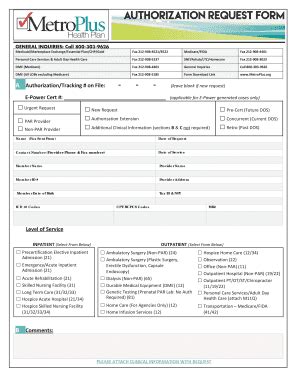
Completing the MetroPlus Prior Authorization Form
The MetroPlus prior authorization form is typically completed by the healthcare provider or their staff. The form requires the following information:
- Section 1: Patient Information
- Patient's name and date of birth
- MetroPlus ID number
- Contact information (address, phone number, etc.)
- Section 2: Healthcare Provider Information
- Healthcare provider's name and credentials
- Practice name and address
- Contact information (phone number, fax number, etc.)
- Section 3: Clinical Information
- Diagnosis and medical condition requiring treatment
- Treatment plan and proposed services
- Medication list and dosages
- Section 4: Medical Records and Test Results
- Relevant medical records and test results supporting the request
- Section 5: Certification
- Healthcare provider's signature and date
Tips for a Successful Submission
To ensure a successful submission, healthcare providers should:
- Complete the form accurately and thoroughly
- Attach all required documents and medical records
- Submit the form well in advance of the proposed treatment date
- Follow up with MetroPlus to confirm receipt and status of the request

Common Mistakes to Avoid
Healthcare providers should avoid the following common mistakes when completing the MetroPlus prior authorization form:
- Incomplete or inaccurate information
- Missing or incomplete medical records
- Insufficient clinical information to support the request
- Failure to submit the form in a timely manner
MetroPlus Prior Authorization Form Status
After submitting the prior authorization form, healthcare providers can check the status of their request through the MetroPlus website or by contacting their representative. The status of the request will be one of the following:
- Approved: The requested service or medication is approved, and the patient can proceed with treatment.
- Denied: The requested service or medication is not approved, and the patient may need to explore alternative options.
- Pended: Additional information or documentation is required to complete the review process.
Appealing a Denied Request
If a prior authorization request is denied, healthcare providers can appeal the decision by submitting additional information or documentation to support the request. The appeal process typically involves:
- Re-review: MetroPlus re-reviews the original request with additional information.
- Peer Review: A peer review is conducted by a medical professional to evaluate the request.

Conclusion
The MetroPlus prior authorization form is a critical document that healthcare providers must complete accurately and thoroughly to ensure that their patients receive necessary care. By understanding the prior authorization process, gathering required information, and avoiding common mistakes, healthcare providers can increase the chances of a successful submission. If a request is denied, appealing the decision may be an option. By following the steps outlined in this guide, healthcare providers can navigate the prior authorization process with ease and ensure that their patients receive the care they need.

Share Your Experience
Have you completed the MetroPlus prior authorization form? Share your experience and tips with us in the comments section below. Your feedback can help others navigate the process more efficiently.
Additional Resources
For more information on the MetroPlus prior authorization process, please visit the MetroPlus website or contact their customer service representative.
What is prior authorization?
+Prior authorization is a process used by health insurance providers to review the medical necessity of certain treatments, procedures, and medications before they are administered or prescribed.
Why is prior authorization required?
+Prior authorization is required to ensure that patients receive necessary care while minimizing unnecessary costs.
How long does the prior authorization process take?
+The prior authorization process typically takes a few days to a week, but can vary depending on the complexity of the request and the availability of required information.