The healthcare landscape in Illinois has undergone significant transformations in recent years, with a growing emphasis on streamlining processes to enhance patient care and reduce administrative burdens. One critical aspect of healthcare management is prior authorization, a process that can be daunting for healthcare providers and patients alike. In this article, we will delve into the world of Meridian prior authorization in Illinois, breaking down the process into five easy steps. Whether you're a healthcare provider looking to simplify your workflow or a patient seeking to understand the process better, this guide is designed to provide you with the insights you need.
Meridian Health Plan of Illinois, Inc., a prominent managed care organization, offers comprehensive health insurance coverage to its members. However, to ensure that patients receive necessary care while controlling healthcare costs, Meridian requires prior authorization for certain medical services and prescription medications. This process can be complex, but understanding the steps involved can significantly ease the burden on both healthcare providers and patients.

Step 1: Determine if Prior Authorization is Required
Before starting the prior authorization process, it's crucial to determine if the medical service or prescription medication requires prior approval from Meridian. This information can typically be found in the patient's health insurance policy documents or by contacting Meridian's customer service directly. Healthcare providers can also check Meridian's website or consult with their billing department to ascertain the requirements.
Step 2: Gather Necessary Information and Documentation
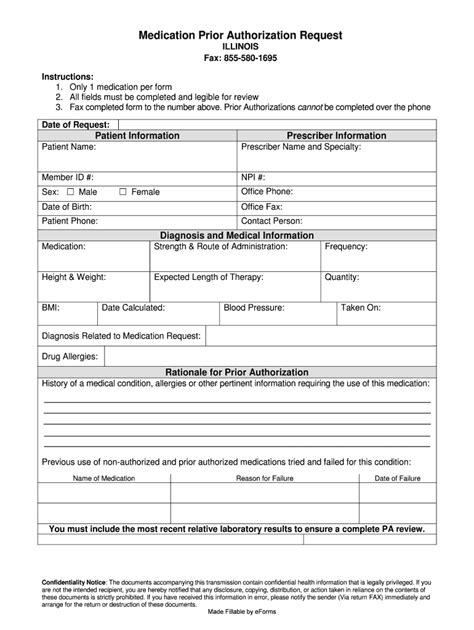
Once it's established that prior authorization is necessary, the next step involves gathering all required information and documentation. This typically includes:
- Patient's medical history and current diagnosis
- Treatment plans and outcomes
- Prescription medication details, including dosage and duration
- Clinical rationale for the requested service or medication
Healthcare providers must ensure that all documentation is accurate, up-to-date, and comprehensive to facilitate a smooth review process.

Step 3: Submit the Prior Authorization Request
With all necessary documentation in hand, the next step is to submit the prior authorization request to Meridian. This can typically be done through Meridian's online portal, by fax, or by mail, depending on the provider's preference and Meridian's guidelines. It's essential to ensure that all required fields are completed accurately and that all supporting documentation is included to avoid delays in the review process.
Step 4: Track and Follow Up on the Request
After submitting the prior authorization request, it's crucial to track its status and follow up as necessary. Meridian typically provides a tracking number or a dedicated portal where providers can check the status of their request. If additional information is required, Meridian will contact the provider directly. Prompt responses to these requests can significantly expedite the review process.
Step 5: Receive and Act on the Decision
Once the review process is complete, Meridian will communicate its decision to the healthcare provider. If the request is approved, the provider can proceed with the prescribed treatment or dispense the medication. If the request is denied, Meridian will provide reasons for the denial, and the provider can discuss alternative treatment options with the patient or appeal the decision if necessary.

Navigating the Meridian prior authorization process in Illinois might seem complex at first, but by following these five easy steps, healthcare providers can ensure a smoother experience for their patients. Understanding the requirements, gathering necessary documentation, submitting accurate requests, tracking the status, and acting on the decision are key to successful prior authorization.
Involving Patients in the Process
While the prior authorization process is primarily managed by healthcare providers, involving patients in the process can lead to better health outcomes and higher patient satisfaction. By keeping patients informed about the status of their prior authorization requests and involving them in discussions about treatment options, providers can foster a more patient-centered approach to healthcare.
The Future of Prior Authorization
The healthcare landscape is continually evolving, with technology playing an increasingly crucial role in streamlining processes like prior authorization. Electronic prior authorization systems and artificial intelligence are being explored as potential solutions to reduce administrative burdens and enhance the patient experience. As these technologies advance, it's likely that the prior authorization process will become more efficient and less daunting for all parties involved.
Conclusion: Simplifying Meridian Prior Authorization
Meridian prior authorization in Illinois doesn't have to be a daunting task. By understanding the steps involved and leveraging technology to streamline the process, healthcare providers can reduce administrative burdens and focus on what matters most – delivering high-quality care to their patients. Whether you're a provider seeking to optimize your workflow or a patient looking to navigate the healthcare system more effectively, this guide has provided you with the insights you need to succeed in the complex world of prior authorization.
Now that you've read through our comprehensive guide to Meridian prior authorization in Illinois, we invite you to share your thoughts and experiences with the process. Have you encountered challenges or successes with prior authorization? What strategies do you think could improve the process for healthcare providers and patients alike? Leave a comment below to join the conversation!
What is prior authorization, and why is it required?
+Prior authorization is a process used by health insurance companies to determine whether a particular medical service or prescription medication is necessary and covered under the patient's policy. It's required to ensure that patients receive necessary care while controlling healthcare costs.
How long does the prior authorization process typically take?
+The length of the prior authorization process can vary depending on the complexity of the request and the efficiency of the healthcare provider in submitting complete and accurate information. Typically, decisions are made within a few days to a couple of weeks.
Can prior authorization requests be submitted electronically?
+Yes, many health insurance companies, including Meridian, offer online portals where healthcare providers can submit prior authorization requests electronically. This can significantly expedite the review process compared to traditional methods like fax or mail.