As a healthcare professional, you understand the importance of obtaining patient authorization for treatment and billing purposes. One crucial document that requires careful completion is the Meridian Authorization Form. In this article, we will explore five ways to complete this form accurately and efficiently.
Completing a Meridian Authorization Form is a crucial step in ensuring that patients receive the necessary treatment while also protecting their personal and financial information. This form serves as a legally binding document that authorizes healthcare providers to disclose patient information to third-party payers, such as insurance companies, for billing and reimbursement purposes. However, with the complexity of healthcare regulations and paperwork, it can be challenging to complete this form correctly.
Fortunately, there are ways to simplify the process and minimize errors. By following the steps outlined in this article, you can ensure that you complete the Meridian Authorization Form accurately and efficiently, saving you time and reducing the risk of rejected claims.
Understanding the Meridian Authorization Form

Before we dive into the five ways to complete the Meridian Authorization Form, it's essential to understand the purpose and structure of this document. The Meridian Authorization Form is a standardized document that requires patients to provide their consent for the disclosure of their protected health information (PHI) to third-party payers.
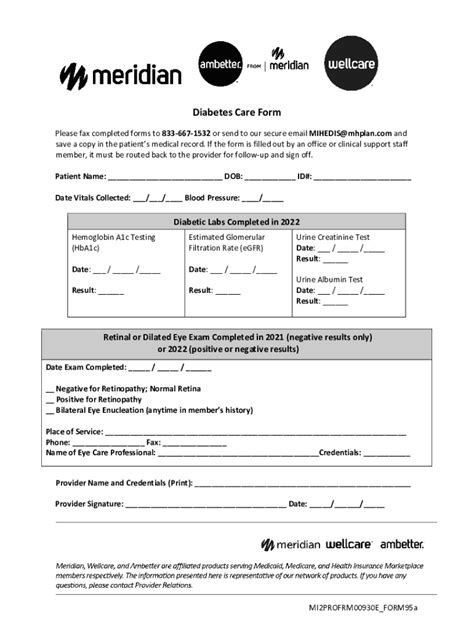
The form typically includes sections for patient demographics, treatment information, and authorization details. It's crucial to complete each section accurately and thoroughly to avoid any delays or rejections in the billing process.
Key Components of the Meridian Authorization Form
- Patient demographics: name, date of birth, address, and contact information
- Treatment information: dates of service, treatment codes, and diagnoses
- Authorization details: patient signature, date, and authorization for disclosure of PHI
5 Ways to Complete a Meridian Authorization Form

Now that we've covered the basics of the Meridian Authorization Form, let's explore five ways to complete this document accurately and efficiently.
1. Review Patient Demographics
The first step in completing the Meridian Authorization Form is to review the patient's demographics. Ensure that the patient's name, date of birth, address, and contact information are accurate and up-to-date. This information is crucial for billing and reimbursement purposes, so it's essential to double-check for any errors.
2. Verify Treatment Information
The next step is to verify the treatment information. Ensure that the dates of service, treatment codes, and diagnoses are accurate and match the patient's medical record. This information is critical for billing and reimbursement purposes, so it's essential to ensure that it's accurate and complete.
3. Obtain Patient Signature
Obtaining the patient's signature is a critical step in completing the Meridian Authorization Form. Ensure that the patient signs and dates the form, indicating their consent for the disclosure of their PHI to third-party payers. This signature serves as a legally binding document, so it's essential to ensure that it's obtained correctly.
4. Ensure Compliance with HIPAA Regulations
The Meridian Authorization Form must comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations. Ensure that the form includes the necessary language and disclosures required by HIPAA, such as the patient's right to revoke authorization and the consequences of disclosure.
5. Review and Verify Form Accuracy
The final step is to review and verify the accuracy of the completed form. Ensure that all sections are complete, and the information is accurate and consistent. Double-check for any errors or omissions, and make any necessary corrections before submitting the form.
Benefits of Accurate Completion

Completing the Meridian Authorization Form accurately and efficiently has numerous benefits for healthcare providers and patients alike. Some of the benefits include:
- Reduced risk of rejected claims
- Faster billing and reimbursement cycles
- Improved patient satisfaction and trust
- Compliance with HIPAA regulations
- Reduced administrative burdens
Common Errors to Avoid
- Incomplete or inaccurate patient demographics
- Missing or incorrect treatment information
- Lack of patient signature or date
- Non-compliance with HIPAA regulations
- Incomplete or inaccurate authorization details
Conclusion
Completing a Meridian Authorization Form is a critical step in the healthcare billing and reimbursement process. By following the five ways outlined in this article, you can ensure that you complete this form accurately and efficiently, reducing the risk of rejected claims and improving patient satisfaction.We hope this article has provided you with valuable insights and tips for completing the Meridian Authorization Form. If you have any questions or concerns, please don't hesitate to reach out.
What is the purpose of the Meridian Authorization Form?
+The Meridian Authorization Form is a standardized document that requires patients to provide their consent for the disclosure of their protected health information (PHI) to third-party payers for billing and reimbursement purposes.
What are the key components of the Meridian Authorization Form?
+The key components of the Meridian Authorization Form include patient demographics, treatment information, and authorization details.
What are the benefits of accurate completion of the Meridian Authorization Form?
+The benefits of accurate completion include reduced risk of rejected claims, faster billing and reimbursement cycles, improved patient satisfaction and trust, compliance with HIPAA regulations, and reduced administrative burdens.