The Fidelis appeal form is a crucial document for individuals who have been denied health insurance benefits or have received an adverse determination from Fidelis Care. Understanding the appeal process and properly completing the appeal form can significantly impact the outcome of your case. In this comprehensive guide, we will walk you through the step-by-step process of completing the Fidelis appeal form, highlighting key information, and providing practical tips to ensure a successful appeal.
Understanding the Fidelis Appeal Process

Before diving into the appeal form, it's essential to understand the overall appeal process. Fidelis Care has a formal appeal process in place, which allows members to dispute adverse determinations or denials of benefits. The appeal process typically involves three levels of review:
- Internal Appeal: The first level of appeal is an internal review by Fidelis Care's appeals department. This review is conducted by a different representative who was not involved in the initial determination.
- External Appeal: If the internal appeal is unsuccessful, members can request an external appeal, which is reviewed by an independent third-party reviewer.
- Final Administrative Determination: The final level of appeal is a review by Fidelis Care's executive director or designee.
Why Is It Important to Complete the Appeal Form Correctly?
Completing the Fidelis appeal form correctly is crucial to ensure that your appeal is reviewed properly and in a timely manner. An incomplete or inaccurate appeal form may lead to delays or even dismissal of your appeal.
Step-by-Step Guide to Completing the Fidelis Appeal Form

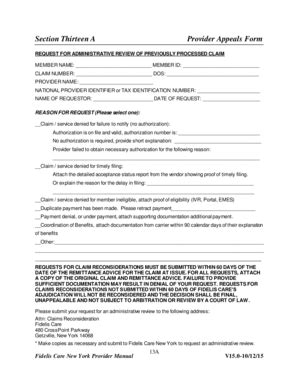
The Fidelis appeal form is typically a multi-page document that requires detailed information about your case. Here's a step-by-step guide to help you complete the form:
- Member Information: Provide your name, member ID, date of birth, and contact information.
- Appeal Reason: Clearly state the reason for your appeal, including the specific service or benefit that was denied or the adverse determination.
- Service Details: Provide detailed information about the service or benefit that was denied, including dates, providers, and medical record numbers.
- Supporting Documentation: Attach all relevant supporting documentation, including medical records, test results, and provider statements.
- Statement of Appeal: Write a clear and concise statement explaining why you disagree with the initial determination and why you believe the service or benefit should be covered.
Tips for Completing the Appeal Form
- Be thorough and accurate: Double-check your information to ensure accuracy and completeness.
- Attach all supporting documentation: Make sure to attach all relevant documents, including medical records and provider statements.
- Clearly state your appeal reason: Use simple language to explain why you are appealing the initial determination.
- Keep a copy of your appeal form: Make a copy of your completed appeal form and supporting documentation for your records.
Common Mistakes to Avoid When Completing the Fidelis Appeal Form

- Inaccurate or incomplete information: Double-check your information to avoid delays or dismissal of your appeal.
- Missing supporting documentation: Ensure that you attach all relevant supporting documentation to support your appeal.
- Unclear or vague appeal reason: Clearly state your appeal reason and why you disagree with the initial determination.
How to Submit Your Fidelis Appeal Form
Once you have completed the appeal form and attached all supporting documentation, you can submit it to Fidelis Care via mail or fax. Make sure to keep a copy of your appeal form and supporting documentation for your records.
What to Expect After Submitting Your Fidelis Appeal Form

After submitting your appeal form, you can expect the following:
- Acknowledgement letter: Fidelis Care will send you an acknowledgement letter confirming receipt of your appeal form.
- Internal appeal review: The appeals department will review your case and make a determination within 30 days.
- External appeal review: If your internal appeal is unsuccessful, you can request an external appeal, which will be reviewed by an independent third-party reviewer.
Additional Tips for a Successful Appeal
- Keep detailed records: Keep a record of all correspondence, including dates, times, and details of conversations.
- Stay organized: Keep all supporting documentation and records organized and easily accessible.
- Seek support: Consider seeking support from a patient advocate or healthcare professional to help navigate the appeal process.
Conclusion
The Fidelis appeal form is a critical document that requires attention to detail and accuracy. By following this step-by-step guide and avoiding common mistakes, you can increase your chances of a successful appeal. Remember to stay organized, keep detailed records, and seek support when needed.
What is the Fidelis appeal process?
+The Fidelis appeal process is a formal process that allows members to dispute adverse determinations or denials of benefits. The process typically involves three levels of review: internal appeal, external appeal, and final administrative determination.
How do I submit my Fidelis appeal form?
+You can submit your Fidelis appeal form via mail or fax. Make sure to keep a copy of your appeal form and supporting documentation for your records.
What should I include in my appeal form?
+Your appeal form should include your member information, appeal reason, service details, and supporting documentation. Make sure to clearly state your appeal reason and why you disagree with the initial determination.