Blue Cross Blue Shield of Alabama (BCBS Alabama) is one of the largest health insurance providers in the state, offering a range of plans to individuals, families, and employers. However, like many insurance providers, BCBS Alabama has a prior authorization process in place to ensure that patients receive medically necessary treatments and services. In this article, we will outline the 5 easy steps for BCBS Alabama prior authorization, making it easier for healthcare providers and patients to navigate the process.

Understanding the Prior Authorization Process
Prior authorization is a process used by health insurance providers to determine whether a treatment or service is medically necessary before it is administered. This process helps ensure that patients receive the most effective and efficient care possible, while also managing healthcare costs. BCBS Alabama requires prior authorization for certain services, including prescription medications, surgeries, and other medical procedures.
Benefits of Prior Authorization
The prior authorization process offers several benefits to healthcare providers, patients, and insurance providers. Some of these benefits include:
- Ensuring that patients receive medically necessary treatments and services
- Reducing healthcare costs by preventing unnecessary treatments and services
- Improving patient outcomes by ensuring that treatments and services are evidence-based
- Enhancing patient safety by reducing the risk of adverse reactions and complications
Step 1: Verify Patient Eligibility
Before starting the prior authorization process, healthcare providers must verify patient eligibility. This involves checking the patient's insurance coverage and ensuring that they are eligible for the requested service or treatment.

To verify patient eligibility, healthcare providers can use the BCBS Alabama website or contact the insurance provider's customer service department. This step is essential in ensuring that patients receive the necessary care and treatments without any unexpected costs or surprises.
Required Information
To verify patient eligibility, healthcare providers will need to provide the following information:
- Patient name and date of birth
- Insurance policy number and group number
- Requested service or treatment
- Date of service or treatment
Step 2: Gather Required Documents
Once patient eligibility has been verified, healthcare providers must gather the required documents to support the prior authorization request. These documents may include:
- Medical records and test results
- Prescription medication lists
- Surgery or treatment plans
- Letters of medical necessity

Healthcare providers must ensure that all required documents are complete and accurate to avoid delays or denials of the prior authorization request.
Tips for Gathering Required Documents
To ensure that the prior authorization process runs smoothly, healthcare providers should:
- Use a checklist to ensure that all required documents are gathered
- Verify that all documents are complete and accurate
- Use electronic health records (EHRs) to streamline the document gathering process
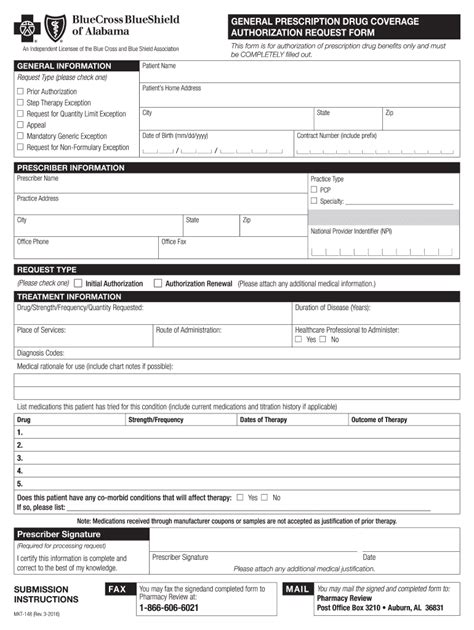
Step 3: Submit the Prior Authorization Request
After gathering the required documents, healthcare providers can submit the prior authorization request to BCBS Alabama. This can be done electronically through the insurance provider's website or by mail.

Healthcare providers must ensure that the prior authorization request is complete and accurate to avoid delays or denials.
Required Information
To submit the prior authorization request, healthcare providers will need to provide the following information:
- Patient name and date of birth
- Insurance policy number and group number
- Requested service or treatment
- Date of service or treatment
- Supporting documents and medical records
Step 4: Review and Follow Up
After submitting the prior authorization request, healthcare providers should review the request to ensure that it is complete and accurate. They should also follow up with BCBS Alabama to ensure that the request is being processed in a timely manner.

Healthcare providers can use the BCBS Alabama website or contact the insurance provider's customer service department to check the status of the prior authorization request.
Tips for Reviewing and Following Up
To ensure that the prior authorization process runs smoothly, healthcare providers should:
- Review the prior authorization request carefully to ensure that it is complete and accurate
- Follow up with BCBS Alabama regularly to ensure that the request is being processed in a timely manner
- Use electronic health records (EHRs) to streamline the review and follow-up process
Step 5: Receive and Review the Prior Authorization Decision
After the prior authorization request has been processed, BCBS Alabama will make a decision regarding the requested service or treatment. Healthcare providers will receive a notification of the decision, which may be an approval, denial, or request for additional information.

Healthcare providers must review the prior authorization decision carefully to ensure that it is accurate and complete.
What to Do If the Request is Denied
If the prior authorization request is denied, healthcare providers can appeal the decision. This involves submitting additional information or documentation to support the request.
Conclusion
The BCBS Alabama prior authorization process may seem complex, but it can be navigated easily by following the 5 easy steps outlined in this article. By verifying patient eligibility, gathering required documents, submitting the prior authorization request, reviewing and following up, and receiving and reviewing the prior authorization decision, healthcare providers can ensure that patients receive the necessary care and treatments without any unexpected costs or surprises.
What is prior authorization?
+Prior authorization is a process used by health insurance providers to determine whether a treatment or service is medically necessary before it is administered.
What is the purpose of prior authorization?
+The purpose of prior authorization is to ensure that patients receive medically necessary treatments and services, while also managing healthcare costs.
How do I submit a prior authorization request to BCBS Alabama?
+You can submit a prior authorization request to BCBS Alabama electronically through the insurance provider's website or by mail.