Healthcare providers and patients alike are no strangers to the complexities of medical billing and insurance claims. One crucial aspect of this process is prior authorization, which can be a daunting task for many. In this article, we will delve into the world of BCBS FEP prior authorization, providing a comprehensive guide to help navigate this often-confusing landscape.
Prior authorization is a critical step in ensuring that patients receive the necessary medical treatment while also controlling healthcare costs. The Blue Cross Blue Shield Federal Employee Program (BCBS FEP) is a prominent health insurance provider that requires prior authorization for certain medical services and treatments. In this article, we will explore the BCBS FEP prior authorization form, its importance, and a step-by-step guide to completing it.
Understanding BCBS FEP Prior Authorization

Prior authorization is a process by which healthcare providers obtain approval from the insurance provider before administering specific medical treatments or services. This step is essential in ensuring that the treatment is medically necessary, cost-effective, and aligns with the patient's coverage plan.
BCBS FEP requires prior authorization for various medical services, including:
- Prescription medications
- Surgical procedures
- Diagnostic tests
- Durable medical equipment
- Outpatient services
Why is BCBS FEP Prior Authorization Important?
Prior authorization plays a vital role in the healthcare system, benefiting both patients and healthcare providers. Some of the key reasons why BCBS FEP prior authorization is important include:
- Ensures medical necessity: Prior authorization helps ensure that patients receive only medically necessary treatments, reducing unnecessary costs and potential harm.
- Controls healthcare costs: By reviewing treatment plans and ensuring that they align with the patient's coverage plan, prior authorization helps control healthcare costs and prevent unnecessary expenses.
- Enhances patient safety: Prior authorization helps identify potential risks and contraindications, ensuring that patients receive safe and effective treatments.
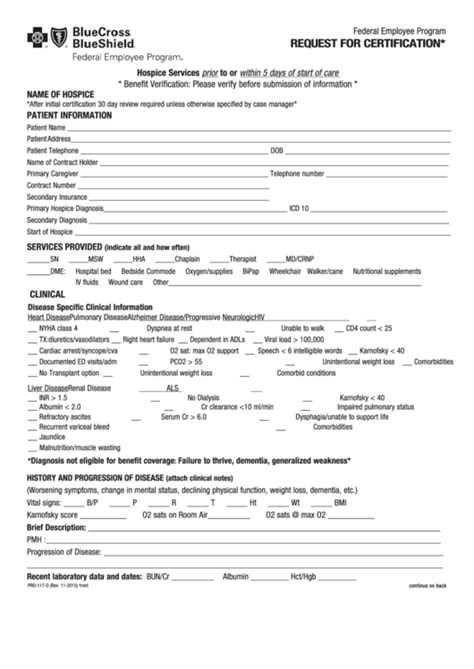
BCBS FEP Prior Authorization Form: A Step-by-Step Guide

Completing the BCBS FEP prior authorization form can be a daunting task, but by following these steps, healthcare providers can ensure a smooth and efficient process.
- Gather necessary information: Before starting the prior authorization process, healthcare providers must gather all necessary information, including:
- Patient demographics
- Medical history
- Current treatment plan
- Diagnosis codes
- Procedure codes
- Determine the type of prior authorization: BCBS FEP requires different types of prior authorization, depending on the medical service or treatment. Healthcare providers must determine the type of prior authorization required for the specific treatment.
- Complete the prior authorization form: The BCBS FEP prior authorization form can be completed online or by phone. Healthcare providers must provide all required information, including patient demographics, medical history, and treatment plans.
- Submit the prior authorization request: Once the form is complete, healthcare providers must submit the prior authorization request to BCBS FEP. This can be done online, by phone, or by mail.
- Receive prior authorization determination: BCBS FEP will review the prior authorization request and provide a determination. This can take several days or weeks, depending on the complexity of the request.
- Appeal prior authorization determination: If the prior authorization request is denied, healthcare providers can appeal the determination. This must be done within a specified timeframe, usually 30 days.
Common Challenges and Solutions
Healthcare providers often face challenges when completing the BCBS FEP prior authorization form. Some common issues include:
- Incomplete or inaccurate information: Ensure that all required information is complete and accurate to avoid delays or denials.
- Incorrect coding: Use correct diagnosis and procedure codes to ensure accurate processing.
- Insufficient medical documentation: Provide detailed medical documentation to support the prior authorization request.
By following these steps and tips, healthcare providers can overcome common challenges and ensure a smooth prior authorization process.
BCBS FEP Prior Authorization Tips and Best Practices

To ensure a successful prior authorization process, healthcare providers should follow these tips and best practices:
- Verify patient eligibility: Ensure that the patient is eligible for coverage before submitting a prior authorization request.
- Use correct coding: Use correct diagnosis and procedure codes to ensure accurate processing.
- Provide detailed medical documentation: Provide detailed medical documentation to support the prior authorization request.
- Follow up on prior authorization requests: Follow up on prior authorization requests to ensure timely processing and determination.
By following these tips and best practices, healthcare providers can streamline the prior authorization process and reduce delays or denials.
Conclusion
The BCBS FEP prior authorization form can be a complex and daunting task, but by following these steps and tips, healthcare providers can ensure a smooth and efficient process. By understanding the importance of prior authorization, gathering necessary information, and completing the form accurately, healthcare providers can help ensure that patients receive the necessary medical treatment while controlling healthcare costs. Remember to follow best practices and tips to overcome common challenges and ensure a successful prior authorization process.
What is BCBS FEP prior authorization?
+BCBS FEP prior authorization is a process by which healthcare providers obtain approval from the insurance provider before administering specific medical treatments or services.
Why is BCBS FEP prior authorization important?
+BCBS FEP prior authorization ensures medical necessity, controls healthcare costs, and enhances patient safety.
How do I complete the BCBS FEP prior authorization form?
+Complete the prior authorization form by gathering necessary information, determining the type of prior authorization, and submitting the request to BCBS FEP.