Prior authorization is a crucial step in the healthcare process, ensuring that patients receive the necessary treatments while also controlling healthcare costs. Molina Healthcare, a leading healthcare organization, requires prior authorization for certain medical services and prescriptions. In this article, we will delve into the Molina Prior Authorization Form, providing a step-by-step guide on how to complete it, the required information, and the benefits of this process.

Understanding the Molina Prior Authorization Form
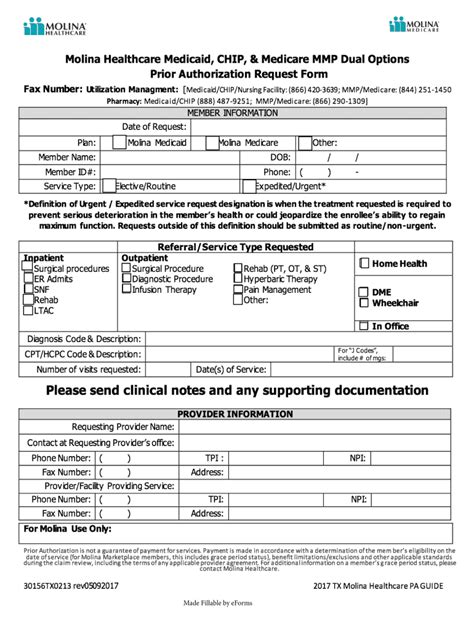
The Molina Prior Authorization Form is a document that healthcare providers must complete to request approval for specific medical services or prescriptions for their patients. This form serves as a tool for Molina Healthcare to assess the medical necessity of the requested treatment and ensure that it aligns with their coverage policies.
Benefits of Prior Authorization
Prior authorization offers several benefits to patients, healthcare providers, and payers. Some of the advantages include:
- Ensures that patients receive medically necessary treatments
- Reduces healthcare costs by avoiding unnecessary procedures
- Improves patient outcomes by ensuring that treatments are evidence-based
- Enhances communication between healthcare providers and payers
- Streamlines the claims process, reducing administrative burdens
Step-by-Step Guide to Completing the Molina Prior Authorization Form
Completing the Molina Prior Authorization Form requires careful attention to detail and accurate information. Here's a step-by-step guide to help healthcare providers complete the form:
- Patient Information: Enter the patient's name, date of birth, and Molina Healthcare member ID number.
- Provider Information: Include the healthcare provider's name, contact information, and National Provider Identifier (NPI) number.
- Service or Prescription Information: Describe the medical service or prescription being requested, including the procedure code, dosage, and frequency.
- Medical Necessity: Explain the medical necessity of the requested treatment, including the patient's diagnosis, symptoms, and treatment history.
- Supporting Documentation: Attach relevant medical records, test results, and other supporting documentation to justify the requested treatment.
- Authorization Request: Specify the type of authorization being requested (e.g., inpatient, outpatient, pharmacy) and the requested dates of service.

Required Information and Supporting Documentation
To ensure that the prior authorization request is processed efficiently, healthcare providers must include all required information and supporting documentation. This may include:
- Patient's medical history and current condition
- Relevant test results and medical records
- Treatment plans and progress notes
- Prescription information, including dosage and frequency
- Supporting documentation from specialists or consultants
Common Mistakes to Avoid
When completing the Molina Prior Authorization Form, healthcare providers should avoid common mistakes, such as:
- Incomplete or inaccurate patient information
- Insufficient medical necessity justification
- Missing or incomplete supporting documentation
- Incorrect procedure codes or billing information

Benefits of Electronic Prior Authorization
Molina Healthcare offers electronic prior authorization, which provides several benefits to healthcare providers, including:
- Streamlined submission process
- Reduced administrative burdens
- Faster processing times
- Improved accuracy and reduced errors
How to Submit the Molina Prior Authorization Form
Healthcare providers can submit the Molina Prior Authorization Form via:
- Mail: Molina Healthcare, [insert address]
- Fax: [insert fax number]
- Electronic submission: through Molina's secure online portal

Conclusion
The Molina Prior Authorization Form is an essential document that ensures patients receive medically necessary treatments while controlling healthcare costs. By following the step-by-step guide and including all required information and supporting documentation, healthcare providers can ensure a smooth and efficient prior authorization process. We encourage healthcare providers to take advantage of electronic prior authorization and to contact Molina Healthcare for any questions or concerns.
We'd love to hear your thoughts! Please share your experiences with the Molina Prior Authorization Form in the comments below. Don't forget to share this article with your colleagues and friends who may benefit from this information.
What is the purpose of the Molina Prior Authorization Form?
+The Molina Prior Authorization Form is used to request approval for specific medical services or prescriptions for patients.
What information is required on the Molina Prior Authorization Form?
+The form requires patient information, provider information, service or prescription information, medical necessity justification, and supporting documentation.
How do I submit the Molina Prior Authorization Form?
+The form can be submitted via mail, fax, or electronic submission through Molina's secure online portal.