Medicaid prior authorization is a crucial step in ensuring that patients receive the necessary medical treatments and services while also managing healthcare costs. For healthcare providers, completing the prior authorization process can be time-consuming and labor-intensive. In this article, we will explore five easy ways to complete Optima Medicaid prior authorization, making it easier for healthcare providers to focus on what matters most - providing quality patient care.
Understanding Optima Medicaid Prior Authorization

Optima Medicaid prior authorization is a process that requires healthcare providers to obtain approval from Optima Health before providing certain medical services or treatments to Medicaid patients. This process helps ensure that patients receive necessary and cost-effective care while also reducing unnecessary medical expenses.
Benefits of Streamlining Prior Authorization

Streamlining the prior authorization process can have numerous benefits for healthcare providers, including:
- Reduced administrative burden and costs
- Improved patient satisfaction and outcomes
- Enhanced communication between healthcare providers and payers
- Increased efficiency and productivity
- Better management of healthcare costs
Ways to Complete Optima Medicaid Prior Authorization
1. Electronic Prior Authorization (ePA)
Electronic prior authorization (ePA) is a digital process that allows healthcare providers to submit prior authorization requests electronically. This method is faster and more efficient than traditional paper-based or phone-based submissions. ePA also reduces the risk of errors and lost or misplaced documents.
- Benefits of ePA:
- Faster turnaround times
- Reduced administrative burden
- Improved accuracy and reduced errors
- Enhanced patient satisfaction
2. Prior Authorization Software
Prior authorization software is a digital tool that helps healthcare providers manage the prior authorization process. This software can automate tasks, such as submitting requests, tracking status, and receiving approvals. Prior authorization software can also integrate with electronic health records (EHRs) and practice management systems (PMS).
- Benefits of prior authorization software:
- Automated tasks and workflows
- Improved efficiency and productivity
- Enhanced visibility and tracking
- Reduced administrative burden
3. Outsourcing Prior Authorization
Outsourcing prior authorization is a viable option for healthcare providers who want to reduce their administrative burden. Third-party vendors can manage the prior authorization process on behalf of healthcare providers, ensuring timely and accurate submissions.
- Benefits of outsourcing prior authorization:
- Reduced administrative burden and costs
- Improved efficiency and productivity
- Enhanced expertise and knowledge
- Better management of prior authorization workflows
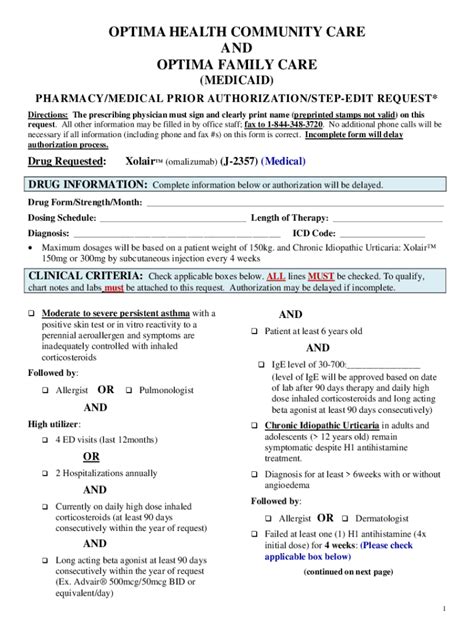
4. Prior Authorization Templates
Prior authorization templates are pre-designed forms that healthcare providers can use to submit prior authorization requests. These templates can help reduce errors and ensure that all necessary information is included.
- Benefits of prior authorization templates:
- Reduced errors and omissions
- Improved accuracy and completeness
- Enhanced efficiency and productivity
- Better management of prior authorization workflows
5. Training and Education
Providing training and education to healthcare staff on the prior authorization process can help improve efficiency and reduce errors. This can include training on Optima Medicaid prior authorization requirements, as well as best practices for submitting requests.
- Benefits of training and education:
- Improved knowledge and understanding
- Enhanced efficiency and productivity
- Reduced errors and omissions
- Better management of prior authorization workflows
Conclusion: Simplifying Optima Medicaid Prior Authorization

Completing Optima Medicaid prior authorization does not have to be a daunting task. By implementing these five easy ways, healthcare providers can streamline the prior authorization process, reduce administrative burden, and improve patient satisfaction. Whether it's through electronic prior authorization, prior authorization software, outsourcing, templates, or training and education, there are numerous options available to simplify the prior authorization process.
We hope this article has provided valuable insights and information on completing Optima Medicaid prior authorization. If you have any questions or comments, please feel free to share them below. Let's work together to simplify the prior authorization process and improve patient care.
What is Optima Medicaid prior authorization?
+Optima Medicaid prior authorization is a process that requires healthcare providers to obtain approval from Optima Health before providing certain medical services or treatments to Medicaid patients.
What are the benefits of streamlining prior authorization?
+Streamlining prior authorization can reduce administrative burden and costs, improve patient satisfaction and outcomes, enhance communication between healthcare providers and payers, increase efficiency and productivity, and better manage healthcare costs.
What is electronic prior authorization (ePA)?
+Electronic prior authorization (ePA) is a digital process that allows healthcare providers to submit prior authorization requests electronically, reducing errors and improving efficiency.