Navigating the complexities of healthcare can be daunting, especially when it comes to dealing with insurance providers. For healthcare professionals and patients alike, understanding the process of appealing a denied claim is crucial. Aetna, one of the largest health insurance companies in the United States, has a specific process for handling appeals from Medicare providers. In this article, we will guide you through the 5 steps to complete an Aetna Medicare provider appeal form, ensuring you understand the process and can effectively advocate for your patients or your practice.
Understanding the Importance of Appeals
Before diving into the steps, it's essential to understand the importance of the appeal process. An appeal is a formal request to review a denied claim or decision made by Aetna. This process is in place to ensure that healthcare providers and patients have a voice in disputing decisions that may affect their care or reimbursement. By understanding the appeal process, you can effectively advocate for your patients and ensure they receive the necessary care.
Step 1: Review the Denial Letter

The first step in the appeal process is to carefully review the denial letter sent by Aetna. This letter will outline the reason for the denial, as well as provide instructions on how to appeal the decision. It's essential to review the letter thoroughly, as it will provide valuable information on the next steps to take.
- Check the denial reason: Understand why the claim was denied. Is it due to a lack of medical necessity, or was the service not covered under the patient's plan?
- Review the appeal instructions: Aetna will provide instructions on how to appeal the decision, including the necessary forms and deadlines.
Step 2: Gather Necessary Documentation
To successfully appeal a denied claim, you will need to gather relevant documentation to support your case.
- Medical records: Collect all relevant medical records, including doctor's notes, test results, and treatment plans.
- Claim details: Gather information about the denied claim, including the date of service, procedure codes, and charges.
- Supporting documentation: Collect any additional documentation that supports the medical necessity of the service, such as letters from specialists or documentation of previous treatments.
Step 3: Complete the Appeal Form
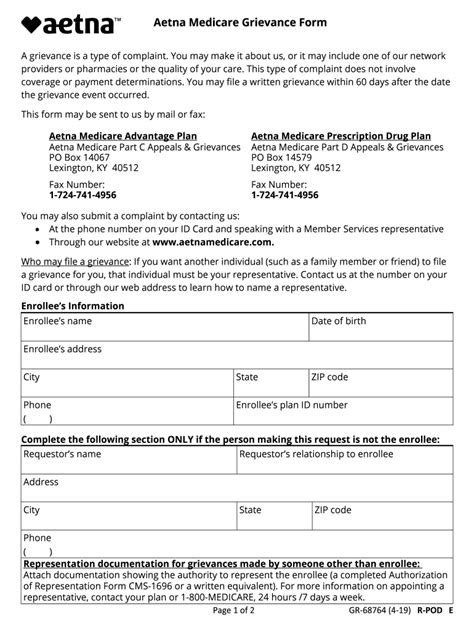
The Aetna Medicare provider appeal form is a critical component of the appeal process.
- Download the form: Visit the Aetna website to download the appeal form. You can also contact Aetna directly to request a form.
- Complete the form: Fill out the form thoroughly, ensuring all required information is provided. This includes patient demographics, claim details, and a clear explanation of why you are appealing the decision.
- Attach supporting documentation: Include all relevant documentation gathered in Step 2.
Step 4: Submit the Appeal
Once the appeal form is complete, it's time to submit it to Aetna.
- Mail the appeal: Send the appeal form and supporting documentation to the address listed on the form.
- Fax the appeal: If you prefer to fax the appeal, use the fax number provided on the form.
- Track the appeal: Keep a record of when the appeal was submitted, including the date and method of submission.
Step 5: Follow Up on the Appeal
After submitting the appeal, it's essential to follow up with Aetna to ensure your appeal is being processed.
- Contact Aetna: Reach out to Aetna's customer service department to confirm receipt of the appeal and inquire about the status.
- Monitor the appeal: Keep track of the appeal's progress, and be prepared to provide additional information if requested.

By following these 5 steps, you can effectively complete an Aetna Medicare provider appeal form and advocate for your patients or your practice. Remember to stay organized, and don't hesitate to reach out to Aetna if you have any questions or concerns throughout the process.
Take Action
We encourage you to share your experiences with the Aetna Medicare provider appeal process in the comments below. If you have any questions or need further guidance, don't hesitate to ask. By working together, we can ensure that healthcare providers and patients receive the necessary support and resources to navigate the complex world of healthcare.
Frequently Asked Questions
What is the deadline for submitting an appeal to Aetna?
+The deadline for submitting an appeal to Aetna varies depending on the type of appeal. Check the denial letter or contact Aetna directly for specific information.
Can I submit an appeal electronically?
+Yes, Aetna offers an electronic appeal submission process. Visit the Aetna website for more information.
How long does the appeal process take?
+The appeal process typically takes 30-60 days, but may vary depending on the complexity of the case.