The West Virginia Medicaid program is designed to provide healthcare coverage to low-income individuals and families. To ensure that medical services and prescriptions are necessary and appropriate, the program requires prior authorization for certain treatments and medications. The prior authorization process is an essential step in ensuring that Medicaid beneficiaries receive the right care while controlling healthcare costs.
West Virginia Medicaid prior authorization is a review process that determines whether a requested medical service or prescription is medically necessary and covered under the Medicaid program. The process involves submitting a prior authorization request form, which is reviewed by a team of medical professionals to ensure that the requested service or medication meets the program's coverage criteria.
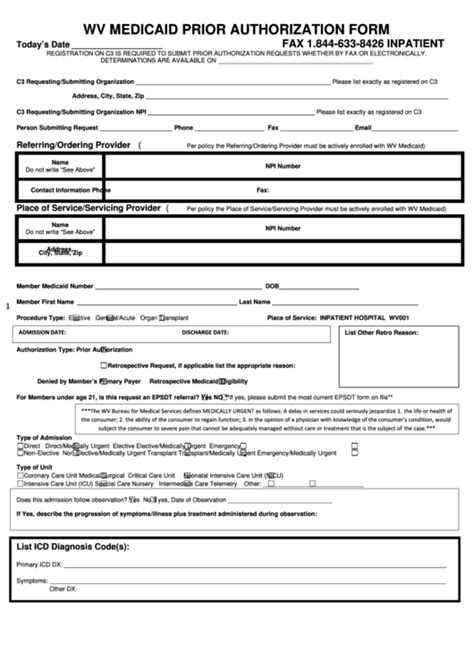
Understanding the WV Medicaid Prior Authorization Form Requirements

To ensure that prior authorization requests are processed efficiently, healthcare providers must submit complete and accurate prior authorization forms. The West Virginia Medicaid program requires the following information to be included on the prior authorization form:
- Patient information, including name, date of birth, and Medicaid ID number
- Healthcare provider information, including name, address, and contact details
- Description of the requested medical service or medication
- Medical justification for the requested service or medication
- Supporting documentation, such as medical records and test results
Types of Prior Authorization Forms
The West Virginia Medicaid program uses different prior authorization forms for different types of services and medications. The most commonly used prior authorization forms include:
- WV Medicaid Prior Authorization Form for Medical Services: This form is used to request prior authorization for medical services, such as surgeries, hospitalizations, and diagnostic tests.
- WV Medicaid Prior Authorization Form for Prescriptions: This form is used to request prior authorization for prescription medications, including brand-name and generic medications.
- WV Medicaid Prior Authorization Form for Durable Medical Equipment (DME): This form is used to request prior authorization for DME, such as wheelchairs, walkers, and oxygen therapy.
The Prior Authorization Process

The prior authorization process typically involves the following steps:
- Submission of the prior authorization form: The healthcare provider submits the completed prior authorization form to the West Virginia Medicaid program.
- Review of the prior authorization form: The West Virginia Medicaid program reviews the prior authorization form to ensure that it is complete and accurate.
- Clinical review: A team of medical professionals reviews the prior authorization form to determine whether the requested service or medication is medically necessary and covered under the Medicaid program.
- Determination: The West Virginia Medicaid program makes a determination on the prior authorization request, which may be approved, denied, or pending additional information.
- Notification: The healthcare provider and the patient are notified of the determination.
Common Reasons for Prior Authorization Denials
The West Virginia Medicaid program may deny a prior authorization request for several reasons, including:
- Lack of medical necessity
- Insufficient documentation
- Non-covered service or medication
- Exceeding frequency or dosage limits
If a prior authorization request is denied, the healthcare provider may appeal the decision by submitting additional information or documentation to support the request.
Benefits of the Prior Authorization Process

The prior authorization process provides several benefits to Medicaid beneficiaries, healthcare providers, and the West Virginia Medicaid program, including:
- Ensuring that medical services and prescriptions are medically necessary and appropriate
- Controlling healthcare costs by reducing unnecessary services and prescriptions
- Improving health outcomes by ensuring that patients receive the right care at the right time
- Reducing administrative burdens by streamlining the prior authorization process
Conclusion
In conclusion, the West Virginia Medicaid prior authorization form requirements are an essential part of the Medicaid program. By understanding the prior authorization process and submitting complete and accurate prior authorization forms, healthcare providers can ensure that Medicaid beneficiaries receive the necessary medical services and prescriptions while controlling healthcare costs.
If you have any questions or concerns about the prior authorization process, please comment below. Share this article with others who may benefit from this information.
What is the purpose of the prior authorization process?
+The prior authorization process is designed to ensure that medical services and prescriptions are medically necessary and covered under the Medicaid program.
What information is required on the prior authorization form?
+The prior authorization form requires patient information, healthcare provider information, description of the requested service or medication, medical justification, and supporting documentation.
What are the common reasons for prior authorization denials?
+Prior authorization requests may be denied due to lack of medical necessity, insufficient documentation, non-covered service or medication, or exceeding frequency or dosage limits.