Navigating the complexities of healthcare can be overwhelming, especially when dealing with denied claims or terminated coverage. Wellcare, a prominent health insurance provider, offers a reconsideration process for members who disagree with certain decisions. This article will delve into the world of Wellcare reconsideration forms, providing a comprehensive guide on how to appeal and increase the chances of a successful outcome.
Understanding the Wellcare Reconsideration Process

The Wellcare reconsideration process is designed to allow members to appeal decisions made by the insurance company. This can include denied claims, terminated coverage, or other adverse determinations. The process typically involves submitting a written request for reconsideration, which is then reviewed by a Wellcare representative. In this section, we'll explore the key aspects of the reconsideration process and what members can expect.
Types of Reconsideration Requests
There are several types of reconsideration requests that can be submitted to Wellcare, including:
- Claim denials: If a claim is denied, members can request reconsideration to have the decision overturned.
- Coverage terminations: If coverage is terminated, members can appeal the decision and request reinstatement.
- Prior authorization denials: If a prior authorization request is denied, members can request reconsideration to have the decision overturned.
Preparing for the Reconsideration Process

Before submitting a reconsideration request, it's essential to prepare and gather the necessary documentation. This may include:
- A clear understanding of the reason for the appeal
- Supporting medical documentation, such as doctor's notes or test results
- A detailed explanation of why the decision should be overturned
- Any relevant correspondence or communication with Wellcare representatives
Gathering Supporting Documentation
Supporting documentation is crucial in the reconsideration process. Members should gather any relevant medical documentation, including:
- Doctor's notes or letters
- Test results or medical records
- Hospital discharge summaries
- Any other relevant medical information
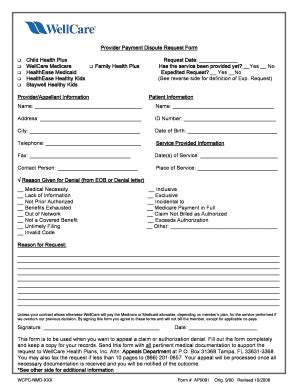
Completing the Wellcare Reconsideration Form

The Wellcare reconsideration form is a critical component of the appeal process. Members should ensure they complete the form accurately and thoroughly, providing all necessary information and supporting documentation.
Section-by-Section Guide
Here's a section-by-section guide to help members complete the Wellcare reconsideration form:
- Section 1: Member Information
- Provide your name, date of birth, and Wellcare member ID
- Section 2: Reason for Appeal
- Clearly explain the reason for the appeal, including the specific decision being appealed
- Section 3: Supporting Documentation
- Attach any supporting medical documentation, including doctor's notes, test results, or medical records
- Section 4: Additional Information
- Provide any additional information or context relevant to the appeal
Submitting the Reconsideration Request

Once the reconsideration form is complete, members should submit it to Wellcare via mail, fax, or online portal. Ensure all necessary documentation is included, and the form is signed and dated.
Timeline for Reconsideration
Wellcare typically has a timeline for reconsideration, which may vary depending on the type of appeal. Members should expect:
- 30-60 days for standard reconsideration requests
- 14-30 days for expedited reconsideration requests
Next Steps and Follow-Up

After submitting the reconsideration request, members should:
- Wait for a response from Wellcare, which may include a request for additional information or documentation
- Follow up with Wellcare representatives to ensure the appeal is being processed
- Review the decision letter carefully and take further action if necessary
Escalating the Appeal
If the reconsideration request is denied, members may have the option to escalate the appeal to an external review organization. This may involve:
- Submitting an external review request to an independent review organization
- Providing additional documentation or information to support the appeal
- Waiting for a decision from the external review organization
What is the Wellcare reconsideration process?
+The Wellcare reconsideration process is a way for members to appeal certain decisions made by the insurance company, such as denied claims or terminated coverage.
How do I complete the Wellcare reconsideration form?
+Members should complete the form accurately and thoroughly, providing all necessary information and supporting documentation. A section-by-section guide is available to help members complete the form.
How long does the reconsideration process take?
+The reconsideration process typically takes 30-60 days for standard requests and 14-30 days for expedited requests.
We hope this comprehensive guide has provided valuable insights into the Wellcare reconsideration process. If you have any further questions or concerns, please don't hesitate to reach out. Share your experiences or ask for advice in the comments below.