Navigating the complex world of healthcare can be overwhelming, especially when it comes to resolving issues with your insurance provider. As an Aetna member, understanding the complaint and appeal process is crucial in ensuring that your concerns are addressed and your rights are protected. In this article, we will delve into the Aetna member complaint and appeal form, explaining the process, benefits, and key information you need to know.
Understanding the Importance of the Complaint and Appeal Process
The complaint and appeal process is a vital component of any healthcare insurance plan, including Aetna. It provides a framework for members to express their concerns, resolve disputes, and seek redress for any grievances they may have. By utilizing this process, members can ensure that their issues are addressed in a fair and timely manner, which is essential for maintaining trust and confidence in their insurance provider.
Benefits of the Complaint and Appeal Process
The complaint and appeal process offers numerous benefits to Aetna members, including:
- Improved customer service: By providing a formal channel for complaints and appeals, Aetna demonstrates its commitment to customer satisfaction and excellence.
- Enhanced transparency: The process ensures that members are informed about the status of their complaints and appeals, promoting transparency and accountability.
- Increased member empowerment: Members have a clear mechanism for expressing their concerns and seeking resolution, which empowers them to take control of their healthcare experience.
- Quality improvement: The complaint and appeal process helps Aetna identify areas for improvement, which can lead to enhanced services and better outcomes for members.
The Aetna Member Complaint and Appeal Form: A Step-by-Step Guide
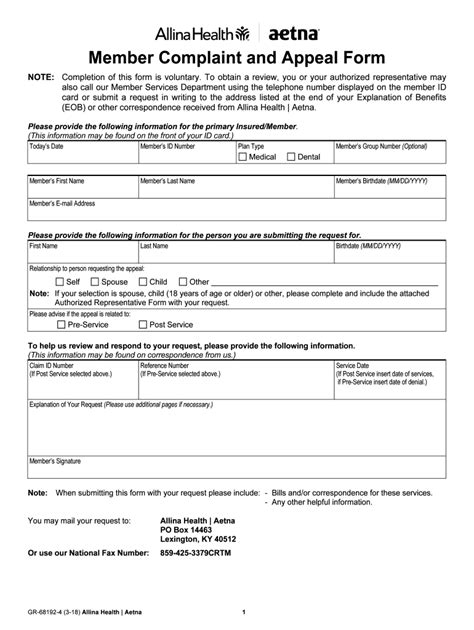
The Aetna member complaint and appeal form is a straightforward document that guides members through the process of submitting a complaint or appeal. Here's a step-by-step explanation of the form:

Section 1: Member Information
The first section of the form requires members to provide their personal and contact information, including:
- Name
- Date of birth
- Policy number
- Address
- Phone number
- Email address
Section 2: Complaint or Appeal Information
In this section, members must provide details about their complaint or appeal, including:
- A clear description of the issue
- The date the issue occurred
- The specific service or benefit in dispute
- Any relevant documentation or evidence supporting the complaint or appeal
Section 3: Resolution Desired
Members must specify the resolution they are seeking, such as:
- Reimbursement for services
- Approval for a specific treatment or service
- Clarification on a policy or procedure
Section 4: Supporting Documentation
Members may need to provide supporting documentation, such as:
- Medical records
- Bills or invoices
- Correspondence with Aetna representatives
Section 5: Signature and Certification
The final section requires members to sign and certify that the information provided is accurate and true.
Key Information and Tips
- Deadlines: Members must submit their complaint or appeal within a specified timeframe, usually 180 days from the date of the dispute.
- Supporting documentation: Members should gather all relevant documentation before submitting their complaint or appeal.
- Clear communication: Members should clearly describe their issue and desired resolution to ensure effective processing.
- Follow-up: Members can follow up on the status of their complaint or appeal by contacting Aetna's customer service department.
Common Mistakes to Avoid
When completing the Aetna member complaint and appeal form, members should avoid the following common mistakes:
- Inaccurate or incomplete information: Ensure that all information provided is accurate and complete to avoid delays or rejection.
- Missing deadlines: Submit the form within the specified timeframe to ensure timely processing.
- Insufficient supporting documentation: Provide all relevant documentation to support the complaint or appeal.
Conclusion and Next Steps
The Aetna member complaint and appeal form is a valuable resource for members seeking to resolve issues with their insurance provider. By understanding the process and following the step-by-step guide, members can ensure that their concerns are addressed and their rights are protected. If you have any further questions or concerns, don't hesitate to reach out to Aetna's customer service department.
We hope this article has provided you with a comprehensive understanding of the Aetna member complaint and appeal form. If you have any feedback or suggestions, please share them with us in the comments section below.
What is the deadline for submitting a complaint or appeal?
+Members must submit their complaint or appeal within 180 days from the date of the dispute.
What supporting documentation do I need to provide?
+Members may need to provide supporting documentation, such as medical records, bills or invoices, and correspondence with Aetna representatives.
How do I follow up on the status of my complaint or appeal?
+Members can follow up on the status of their complaint or appeal by contacting Aetna's customer service department.