Prior authorization is a crucial process in the healthcare system, ensuring that patients receive necessary treatments while controlling healthcare costs. However, it can be a time-consuming and frustrating experience for healthcare providers, especially when dealing with multiple health plans. Tufts Health Plan, a reputable health insurance provider in Massachusetts, has its own prior authorization process. In this article, we will discuss five ways to simplify the Tufts Health Plan prior authorization process, making it more efficient for healthcare providers and ultimately benefiting patients.
Understanding the Prior Authorization Process
Before diving into simplification strategies, it's essential to understand the prior authorization process. Prior authorization, also known as pre-authorization or pre-certification, is a process where healthcare providers obtain approval from a health plan before providing specific treatments or services to patients. This process aims to ensure that the treatment is medically necessary, cost-effective, and aligned with the health plan's guidelines.
1. Familiarize Yourself with Tufts Health Plan's Prior Authorization Requirements

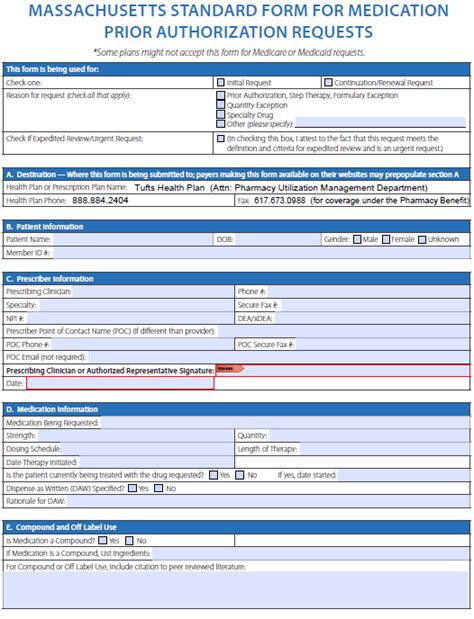
To simplify the prior authorization process, healthcare providers should familiarize themselves with Tufts Health Plan's requirements. This includes understanding the types of services and treatments that require prior authorization, the necessary documentation, and the submission process. Tufts Health Plan provides a comprehensive prior authorization guide on their website, which healthcare providers can consult to ensure compliance.
Simplification Strategies
2. Utilize Electronic Prior Authorization Systems
Benefits of Electronic Prior Authorization Systems
Electronic prior authorization systems can significantly simplify the process by reducing paperwork, minimizing errors, and increasing efficiency. These systems enable healthcare providers to submit prior authorization requests electronically, receive instant approval or denial notifications, and track the status of their requests. Tufts Health Plan has partnered with electronic prior authorization vendors, such as CoverMyMeds and Surescripts, to offer a more streamlined process.
Benefits of Electronic Prior Authorization Systems:
• Reduced paperwork and administrative burdens • Minimized errors and improved accuracy • Increased efficiency and faster approval times • Improved communication and transparency
3. Leverage Prior Authorization Tools and Resources
Prior Authorization Tools and Resources
Tufts Health Plan offers various tools and resources to help healthcare providers navigate the prior authorization process. These include:
• Prior authorization guides and manuals • Online prior authorization submission systems • Phone and email support • Webinars and training sessions
By leveraging these tools and resources, healthcare providers can reduce the complexity of the prior authorization process and ensure compliance with Tufts Health Plan's requirements.
4. Implement a Prior Authorization Workflow
Prior Authorization Workflow
Implementing a prior authorization workflow can help healthcare providers manage the process more efficiently. This includes:
• Designating a prior authorization coordinator or team • Establishing a prior authorization submission process • Tracking and following up on prior authorization requests • Communicating with patients and providers about prior authorization status
By streamlining the prior authorization workflow, healthcare providers can reduce administrative burdens and improve patient satisfaction.
5. Stay Up-to-Date with Tufts Health Plan's Prior Authorization Policy Changes
Importance of Staying Up-to-Date
Tufts Health Plan's prior authorization policies and procedures can change over time. Healthcare providers must stay up-to-date with these changes to ensure compliance and avoid delays or denials. Tufts Health Plan provides regular updates on their website, and healthcare providers can also subscribe to their newsletter or attend webinars to stay informed.
Conclusion
Simplifying the Tufts Health Plan prior authorization process requires a combination of understanding the requirements, leveraging electronic systems and tools, implementing efficient workflows, and staying up-to-date with policy changes. By adopting these strategies, healthcare providers can reduce administrative burdens, improve patient satisfaction, and ultimately deliver better care.

Engage with Us
We hope this article has provided valuable insights into simplifying the Tufts Health Plan prior authorization process. Share your thoughts and experiences with us in the comments section below. Have you implemented any of these strategies in your practice? What challenges have you faced, and how have you overcome them? Your feedback will help us create more informative and engaging content.
FAQ Section
What is prior authorization, and why is it necessary?
+Prior authorization is a process where healthcare providers obtain approval from a health plan before providing specific treatments or services to patients. It ensures that the treatment is medically necessary, cost-effective, and aligned with the health plan's guidelines.
How can I check the status of my prior authorization request?
+You can check the status of your prior authorization request by logging into Tufts Health Plan's online portal or by contacting their customer service department.
What are the benefits of using electronic prior authorization systems?
+The benefits of using electronic prior authorization systems include reduced paperwork, minimized errors, increased efficiency, and improved communication and transparency.