Receiving the necessary medication to manage a health condition can be a challenging and frustrating experience, especially when it comes to navigating the complexities of insurance coverage. Tricare, a health care program sponsored by the US Department of Defense, provides coverage for military personnel, veterans, and their families. However, some medications may require prior authorization, which can add an extra layer of complexity to the process. In this article, we will break down the 5 steps to Tricare prior authorization for medication, making it easier for you to understand and navigate the process.
Understanding Tricare Prior Authorization

Tricare prior authorization is a process that requires your healthcare provider to obtain approval from Tricare before prescribing certain medications. This is typically done to ensure that the medication is medically necessary and that you have tried other treatment options before moving to a more expensive or specialized medication. The prior authorization process is in place to help control costs and ensure that you receive the most effective treatment for your condition.
Why is Tricare Prior Authorization Required?
Tricare prior authorization is required for several reasons:
- To ensure that the medication is medically necessary and that you have tried other treatment options before moving to a more expensive or specialized medication.
- To control costs by ensuring that you are receiving the most cost-effective treatment for your condition.
- To ensure that you are receiving safe and effective treatment for your condition.
Step 1: Verify Tricare Coverage

Before starting the prior authorization process, it's essential to verify that your medication is covered under Tricare. You can do this by:
- Checking the Tricare website for a list of covered medications.
- Contacting Tricare customer service to ask about coverage for your specific medication.
- Reviewing your Tricare policy documents to see if your medication is listed as a covered benefit.
What to Do if Your Medication is Not Covered
If your medication is not covered under Tricare, you may need to explore alternative treatment options or file an appeal to have your medication covered.
Step 2: Gather Required Documents

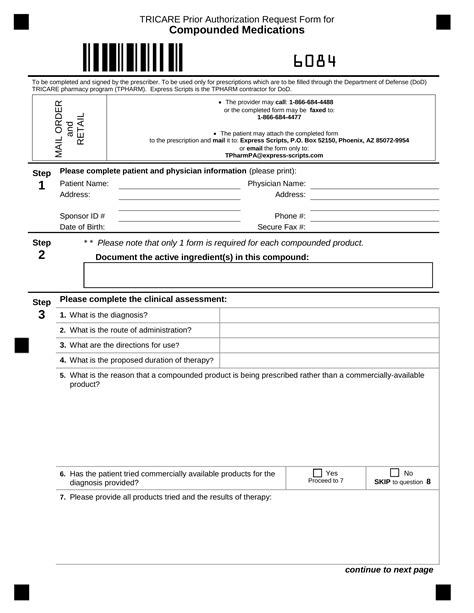
To initiate the prior authorization process, your healthcare provider will need to gather the following documents:
- Your medical records, including a diagnosis and treatment plan.
- A list of medications you have tried in the past and their effectiveness.
- Any relevant test results or medical imaging.
What to Expect During the Document Collection Process
During the document collection process, your healthcare provider may need to contact you to gather additional information or clarify specific details. Be prepared to provide detailed information about your medical history and treatment plan.
Step 3: Submit the Prior Authorization Request

Once your healthcare provider has gathered all the necessary documents, they will submit a prior authorization request to Tricare. This request will include all the relevant information, including your medical history, treatment plan, and medication information.
What to Expect During the Prior Authorization Review Process
During the prior authorization review process, Tricare will review your request to determine if your medication is medically necessary and if you have tried other treatment options. This process typically takes a few days to a week, but can take longer in some cases.
Step 4: Receive Prior Authorization Approval or Denial

Once Tricare has reviewed your prior authorization request, they will notify your healthcare provider of their decision. If your request is approved, you will be able to receive your medication. If your request is denied, you may need to appeal the decision or explore alternative treatment options.
What to Do if Your Prior Authorization Request is Denied
If your prior authorization request is denied, you may need to:
- Appeal the decision by providing additional information or clarification.
- Explore alternative treatment options that are covered under Tricare.
- File a grievance with Tricare if you feel that the decision was unfair or not in your best interest.
Step 5: Maintain Prior Authorization Approval

Once you have received prior authorization approval, you will need to maintain it by:
- Adhering to your treatment plan and medication regimen.
- Attending follow-up appointments with your healthcare provider.
- Providing updates to Tricare if your condition changes or if you experience any side effects.
What to Expect During the Maintenance Process
During the maintenance process, your healthcare provider will work closely with you to ensure that you are receiving the best possible treatment for your condition. They will also communicate with Tricare to ensure that your prior authorization approval is maintained.
Now that you have completed the 5 steps to Tricare prior authorization for medication, you can feel more confident in your ability to navigate the process. Remember to stay informed, ask questions, and advocate for yourself throughout the process.
If you have any questions or concerns about Tricare prior authorization, please don't hesitate to reach out to us. We're here to help!
What is Tricare prior authorization?
+Tricare prior authorization is a process that requires your healthcare provider to obtain approval from Tricare before prescribing certain medications.
Why is Tricare prior authorization required?
+Tricare prior authorization is required to ensure that the medication is medically necessary, to control costs, and to ensure that you are receiving safe and effective treatment for your condition.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you may need to appeal the decision, explore alternative treatment options, or file a grievance with Tricare.