The healthcare system can be overwhelming, especially when it comes to navigating the complexities of insurance coverage and prior authorizations. For individuals covered by Tricare East, understanding the prior authorization process is crucial to ensuring smooth and uninterrupted access to medical care. In this article, we will delve into the world of Tricare East prior authorization forms, providing a comprehensive guide to help you navigate this often-daunting process.

Tricare East is one of the regional contractors under the Tricare program, specifically serving the eastern United States. One of the key aspects of Tricare East, like many health insurance plans, is the requirement for prior authorization for certain medical services and prescriptions. This process is designed to ensure that patients receive medically necessary care while also managing healthcare costs.
What is a Prior Authorization?
Prior authorization, often abbreviated as PA, is a requirement from your health insurance provider that your doctor must obtain before prescribing certain medications, undergoing specific treatments, or accessing particular medical services. This process involves your healthcare provider submitting a request to your insurance company, detailing the medical necessity of the proposed treatment or medication. The insurance company then reviews this request to determine whether it aligns with their coverage policies and medical guidelines.

Why is Prior Authorization Necessary?
Prior authorization serves several purposes:
- Ensures Medical Necessity: It verifies that the prescribed treatment or medication is medically necessary for the patient's condition, aligning with established clinical guidelines.
- Manages Healthcare Costs: By reviewing and approving requests before services are rendered, insurers can better manage costs and avoid unnecessary expenditures.
- Enhances Patient Safety: Prior authorization can help prevent inappropriate use of medications or treatments, thus enhancing patient safety.
How to Obtain a Tricare East Prior Authorization Form
To initiate the prior authorization process with Tricare East, your healthcare provider will typically need to submit a request. Here’s how you can obtain the necessary form:
- Contact Your Healthcare Provider: Reach out to your doctor or healthcare provider and explain your need for prior authorization. They will guide you through the next steps.
- Access the Tricare East Website: You can visit the official Tricare East website to find the necessary forms and guidelines for prior authorization.
- Tricare East Customer Service: If you're unsure about where to start or need assistance with the process, contacting Tricare East's customer service can provide you with the information and forms you need.

Filling Out the Tricare East Prior Authorization Form
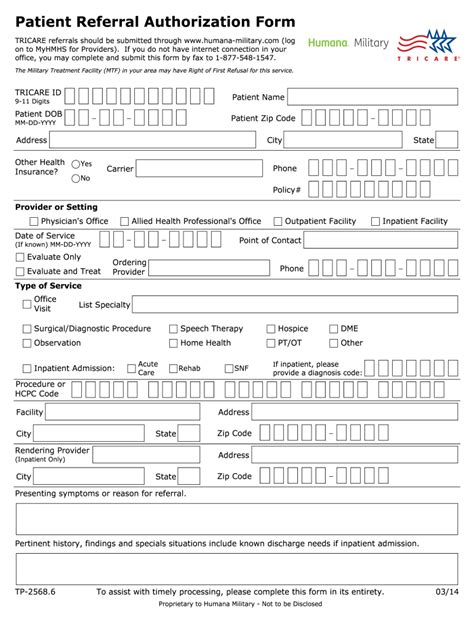
When filling out the prior authorization form, it's essential to ensure that all required information is accurately and completely provided. This typically includes:
- Patient Information: Full name, date of birth, and Tricare ID number.
- Medical Condition: A clear description of the medical condition or diagnosis requiring treatment.
- Proposed Treatment or Medication: Detailed information about the prescribed treatment or medication, including dosage and frequency.
- Clinical Rationale: An explanation from your healthcare provider justifying the medical necessity of the proposed treatment.
Submitting the Prior Authorization Request
Once the form is completed, your healthcare provider will submit it to Tricare East for review. The submission process may vary, but it often involves faxing or electronically submitting the form along with any required supporting documents, such as medical records or test results.

What to Expect After Submission
After Tricare East receives the prior authorization request, they will review it to determine whether the proposed treatment or medication aligns with their coverage policies and medical guidelines. This process can take several days to a few weeks. You or your healthcare provider will be notified of the decision.
Tips for a Smooth Prior Authorization Process
To ensure a smooth and efficient prior authorization process:
- Start Early: Allow ample time for the review process to avoid delays in treatment.
- Provide Complete Information: Ensure that all required information is accurately and completely provided on the form.
- Follow Up: If necessary, follow up with Tricare East to check on the status of your request.

Navigating the prior authorization process with Tricare East can seem daunting, but understanding the requirements and being prepared can make all the difference. By following the guidelines outlined in this article and maintaining open communication with your healthcare provider and Tricare East, you can ensure that you receive the necessary medical care without unnecessary delays.
We hope this guide has been informative and helpful. If you have any further questions or experiences with the Tricare East prior authorization process, please share them in the comments below. Your insights can help others navigate this complex healthcare landscape.
What is the purpose of prior authorization with Tricare East?
+Prior authorization with Tricare East is required to ensure that prescribed treatments or medications are medically necessary and align with established clinical guidelines, thereby managing healthcare costs and enhancing patient safety.
How do I obtain a Tricare East prior authorization form?
+You can obtain the Tricare East prior authorization form by contacting your healthcare provider, visiting the Tricare East website, or reaching out to Tricare East's customer service.
What information is required on the Tricare East prior authorization form?
+The form requires patient information, a clear description of the medical condition, details about the proposed treatment or medication, and a clinical rationale from your healthcare provider justifying the medical necessity of the proposed treatment.