Understanding the Importance of Prior Authorization for Dupixent

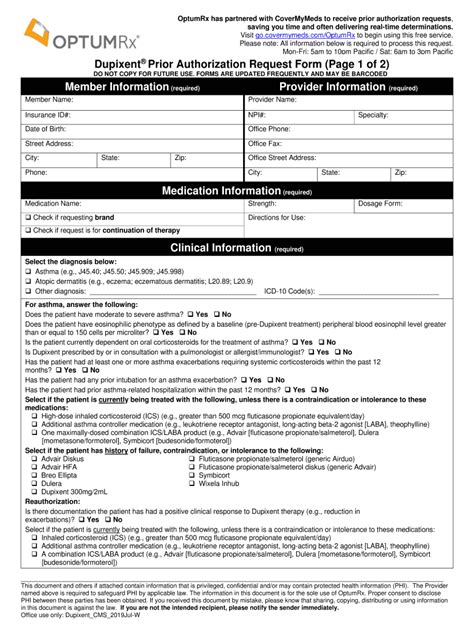
In the world of healthcare, prior authorization has become a crucial step in ensuring that patients receive the necessary medications while also controlling costs. For patients prescribed Dupixent, a medication used to treat moderate-to-severe atopic dermatitis and asthma, obtaining prior authorization from their insurance provider is often required. In this article, we will delve into the specifics of filling out the OptumRx Dupixent prior auth form, a crucial document that must be completed accurately to ensure timely approval.
Why Prior Authorization is Necessary
Prior authorization is a process by which healthcare providers obtain approval from a patient's insurance provider before prescribing a specific medication. This process helps ensure that the prescribed medication is medically necessary and that the patient meets the insurance provider's coverage criteria. In the case of Dupixent, prior authorization is often required due to the medication's high cost and potential side effects.
Step 1: Gather Required Information

Before starting the prior authorization process, it is essential to gather all required information. This includes:
- Patient demographics, such as name, date of birth, and insurance ID number
- Diagnosis and medical history
- Medication history, including previous treatments and dosages
- Current treatment plan and dosage
- ICD-10 code for the patient's condition
Having this information readily available will help streamline the prior authorization process.
Step 2: Complete Section 1 of the OptumRx Dupixent Prior Auth Form
Section 1 of the OptumRx Dupixent prior auth form requires demographic information about the patient. This includes:
- Patient name and date of birth
- Insurance ID number and group number
- Primary care physician's name and contact information
It is essential to ensure that all information is accurate and up-to-date to avoid delays in the prior authorization process.
Step 3: Complete Section 2 of the OptumRx Dupixent Prior Auth Form

Section 2 of the OptumRx Dupixent prior auth form requires information about the patient's medical history and current treatment plan. This includes:
- Diagnosis and ICD-10 code for the patient's condition
- Medication history, including previous treatments and dosages
- Current treatment plan and dosage
- Reason for requesting Dupixent
It is crucial to provide detailed information about the patient's medical history to ensure that the insurance provider understands the necessity of the medication.
Step 4: Attach Supporting Documentation
In addition to completing the prior auth form, it is essential to attach supporting documentation, such as:
- Medical records and lab results
- Treatment plans and progress notes
- Letters of medical necessity
This documentation helps support the request for prior authorization and ensures that the insurance provider has all necessary information to make an informed decision.
Step 5: Submit the Prior Auth Form

Once the prior auth form is complete, and supporting documentation is attached, it is ready for submission. The form can be submitted via fax, email, or online portal, depending on the insurance provider's requirements.
Tips for a Smooth Prior Authorization Process
To ensure a smooth prior authorization process, it is essential to:
- Complete the form accurately and thoroughly
- Attach all required supporting documentation
- Submit the form in a timely manner
- Follow up with the insurance provider to ensure receipt of the form and to address any questions or concerns
By following these steps and tips, healthcare providers can ensure a smooth prior authorization process for their patients prescribed Dupixent.
Conclusion
The OptumRx Dupixent prior auth form is a crucial document that requires accurate and thorough completion. By gathering required information, completing the form, attaching supporting documentation, and submitting it in a timely manner, healthcare providers can ensure a smooth prior authorization process for their patients. If you have any questions or concerns about the prior authorization process, please do not hesitate to reach out to your insurance provider or healthcare team.
What is prior authorization?
+Prior authorization is a process by which healthcare providers obtain approval from a patient's insurance provider before prescribing a specific medication.
Why is prior authorization necessary for Dupixent?
+Prior authorization is necessary for Dupixent due to the medication's high cost and potential side effects.
How long does the prior authorization process take?
+The prior authorization process typically takes 3-5 business days, but can vary depending on the insurance provider and complexity of the request.