The world of healthcare can be complex and overwhelming, especially when it comes to navigating the process of prior authorization. For patients, understanding the prior authorization process can be a daunting task, and for healthcare providers, managing the paperwork and bureaucracy can be time-consuming and frustrating. That's where Myameriben comes in – a solution designed to simplify the prior authorization process, making it easier for patients and healthcare providers to access the care they need.
For patients, prior authorization can be a source of anxiety and uncertainty. Will their treatment be approved? How long will it take? What if it's denied? These questions can weigh heavily on patients, who may already be dealing with the stress of a medical condition. By streamlining the prior authorization process, Myameriben aims to alleviate some of this burden, providing patients with a clearer understanding of what to expect and when.

What is Prior Authorization?
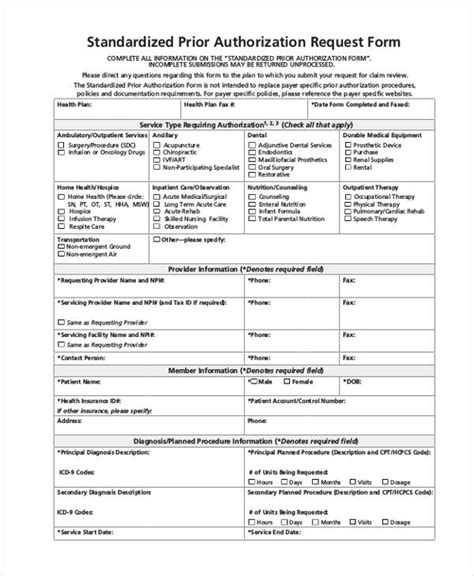
Prior authorization is a process used by health insurance companies to determine whether a particular treatment or medication is medically necessary. The goal of prior authorization is to ensure that patients receive safe and effective care, while also controlling healthcare costs. However, the process can be time-consuming and may require significant paperwork and documentation.
How Does Prior Authorization Work?
The prior authorization process typically involves several steps:
- The patient's healthcare provider submits a request for prior authorization to the insurance company.
- The insurance company reviews the request to determine whether the treatment is medically necessary.
- If additional information is needed, the insurance company may request further documentation from the patient's healthcare provider.
- Once the request is approved or denied, the insurance company notifies the patient's healthcare provider.
The Benefits of Myameriben
Myameriben is designed to simplify the prior authorization process, making it easier for patients and healthcare providers to navigate. Some of the benefits of using Myameriben include:
- Streamlined paperwork: Myameriben automates the prior authorization process, reducing the need for paperwork and minimizing the risk of errors.
- Faster approval times: By simplifying the process, Myameriben can help reduce the time it takes for prior authorization requests to be approved.
- Improved communication: Myameriben provides a clear and transparent process, keeping patients and healthcare providers informed every step of the way.

How to Use Myameriben
Using Myameriben is a straightforward process. Here's a step-by-step guide:
- Create an account: Patients and healthcare providers can create an account on the Myameriben website.
- Submit a request: Once logged in, patients and healthcare providers can submit a prior authorization request.
- Track the status: Myameriben provides a clear and transparent process, allowing patients and healthcare providers to track the status of their request.
Common Challenges and Solutions
While Myameriben is designed to simplify the prior authorization process, there may still be challenges that arise. Here are some common issues and solutions:
- Incomplete paperwork: One of the most common challenges is incomplete paperwork. To avoid this, patients and healthcare providers should ensure that all necessary documentation is submitted with the prior authorization request.
- Denied requests: If a prior authorization request is denied, patients and healthcare providers should review the reasons for the denial and resubmit the request with any additional necessary information.

Conclusion
Navigating the prior authorization process can be a complex and overwhelming task, but with Myameriben, patients and healthcare providers can simplify the process and access the care they need more easily. By understanding the benefits and challenges of prior authorization, patients and healthcare providers can work together to ensure that patients receive the best possible care.
Final Thoughts
The prior authorization process is an essential part of the healthcare system, but it can be a source of frustration for patients and healthcare providers. By using Myameriben, patients and healthcare providers can streamline the process, reduce paperwork, and improve communication. Whether you're a patient or a healthcare provider, Myameriben is here to help you navigate the prior authorization process with ease.

What is prior authorization?
+Prior authorization is a process used by health insurance companies to determine whether a particular treatment or medication is medically necessary.
How does Myameriben work?
+Myameriben is a solution designed to simplify the prior authorization process, making it easier for patients and healthcare providers to access the care they need.
What are the benefits of using Myameriben?
+The benefits of using Myameriben include streamlined paperwork, faster approval times, and improved communication.