The process of obtaining prior authorization for medical treatments or services can be complex and time-consuming. Molina Healthcare, a leading healthcare provider, requires a prior authorization request form to be completed and submitted before certain medical procedures or treatments can be approved. In this article, we will provide a step-by-step guide on how to complete the Molina prior authorization request form, highlighting the importance of accuracy and completeness in the process.
Understanding the Importance of Prior Authorization

Prior authorization is a process used by healthcare providers to ensure that medical treatments or services are medically necessary and meet specific criteria before they are approved. This process helps to control healthcare costs, prevent unnecessary treatments, and ensure that patients receive high-quality care. For Molina Healthcare, prior authorization is an essential step in ensuring that patients receive the necessary medical care while minimizing costs.
Step 1: Gathering Required Information

Before completing the Molina prior authorization request form, it is essential to gather all required information. This includes:
- Patient demographics, including name, date of birth, and contact information
- Medical history, including diagnosis and treatment information
- Provider information, including name, contact information, and National Provider Identifier (NPI)
- Treatment or service information, including procedure codes and descriptions
- Supporting documentation, including medical records and test results
Step 1.1: Verifying Patient Eligibility
Verifying patient eligibility is a critical step in the prior authorization process. This involves checking the patient's coverage status, including their policy number, coverage dates, and any specific coverage restrictions.
Step 1.2: Identifying Required Documents
Identifying required documents is essential to ensure that the prior authorization request is complete and accurate. This may include medical records, test results, and other supporting documentation.
Step 2: Completing the Prior Authorization Request Form

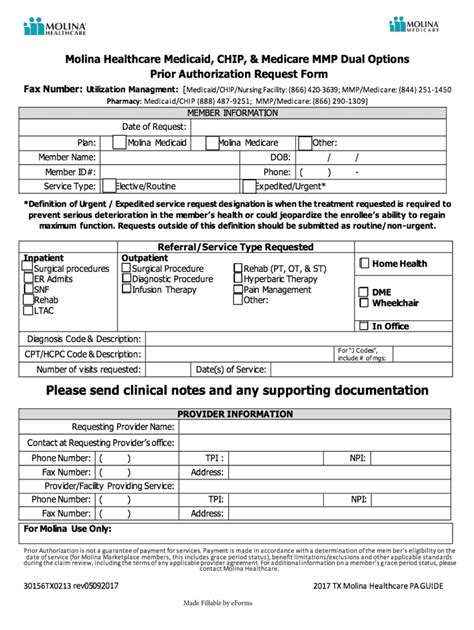
The Molina prior authorization request form is a standardized document that requires specific information to be completed. This includes:
- Patient demographics and medical history
- Provider information and treatment or service details
- Supporting documentation, including medical records and test results
- Certification and authorization statements
Step 2.1: Completing Patient Demographics and Medical History
Completing patient demographics and medical history is essential to ensure that the prior authorization request is accurate and complete. This includes providing detailed information about the patient's medical condition, including diagnosis and treatment information.
Step 2.2: Completing Provider Information and Treatment or Service Details
Completing provider information and treatment or service details is critical to ensure that the prior authorization request is accurate and complete. This includes providing detailed information about the provider, including their name, contact information, and NPI, as well as the treatment or service being requested.
Step 3: Submitting the Prior Authorization Request Form

Once the prior authorization request form is complete, it must be submitted to Molina Healthcare for review and approval. This can be done via fax, email, or online portal.
Step 3.1: Tracking the Prior Authorization Request
Tracking the prior authorization request is essential to ensure that the request is processed efficiently and effectively. This includes checking the status of the request and following up with Molina Healthcare as necessary.
Conclusion: Efficiently Navigating the Prior Authorization Process

In conclusion, completing the Molina prior authorization request form requires attention to detail, accuracy, and completeness. By following the steps outlined in this guide, healthcare providers can efficiently navigate the prior authorization process, ensuring that patients receive the necessary medical care while minimizing costs.
We encourage you to share your experiences with the Molina prior authorization request form in the comments section below. Have you encountered any challenges or difficulties with the process? Do you have any tips or advice for healthcare providers completing the form? Share your thoughts and help others navigate the prior authorization process.
What is prior authorization?
+Prior authorization is a process used by healthcare providers to ensure that medical treatments or services are medically necessary and meet specific criteria before they are approved.
Why is prior authorization important?
+Prior authorization helps to control healthcare costs, prevent unnecessary treatments, and ensure that patients receive high-quality care.
What information is required to complete the Molina prior authorization request form?
+The required information includes patient demographics, medical history, provider information, treatment or service details, and supporting documentation.