Molina Healthcare is a prominent health insurance provider in the United States, serving millions of individuals and families across the country. As a part of their commitment to delivering quality healthcare services, Molina requires prior authorization for certain medical procedures and medications to ensure that their members receive necessary and cost-effective care. In this article, we will delve into the intricacies of filling out the Molina prior authorization form and provide guidance on navigating this often-complex process.

Understanding the Molina Prior Authorization Form
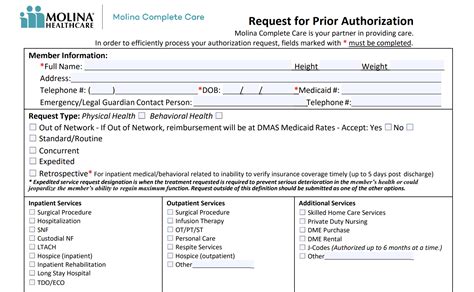
The Molina prior authorization form is a crucial document that healthcare providers must complete to obtain approval for specific medical treatments or services. The form typically requires detailed information about the patient's condition, the proposed treatment or medication, and the rationale behind the chosen course of action.
Key Components of the Molina Prior Authorization Form
To successfully fill out the Molina prior authorization form, healthcare providers must ensure that they provide accurate and comprehensive information. Some of the key components of the form include:
- Patient demographics and insurance information
- Diagnosis and medical history
- Proposed treatment or medication
- Clinical rationale and supporting documentation
- Healthcare provider's signature and contact information
5 Ways to Fill Out the Molina Prior Authorization Form
Filling out the Molina prior authorization form can be a daunting task, especially for healthcare providers who are new to the process. Here are five ways to simplify the process and increase the chances of successful authorization:
1. Familiarize Yourself with Molina's Prior Authorization Requirements
Before starting the prior authorization process, healthcare providers should review Molina's requirements and guidelines. This includes understanding the types of treatments and services that require prior authorization, the necessary documentation, and the expected timelines for approval.
2. Gather All Necessary Information and Documentation
To complete the prior authorization form accurately, healthcare providers must gather all relevant information and documentation, including:
- Patient medical records and test results
- Prescription information and medication lists
- Consultation reports and specialist recommendations
- Clinical notes and progress reports
3. Complete the Form Accurately and Thoroughly
Healthcare providers should take the time to complete the prior authorization form accurately and thoroughly, ensuring that all required fields are filled out and supporting documentation is attached. Incomplete or inaccurate forms may lead to delays or denials.
4. Use Molina's Online Prior Authorization Portal
Molina offers an online prior authorization portal that allows healthcare providers to submit requests electronically. This portal can streamline the process, reduce paperwork, and improve turnaround times.
5. Follow Up with Molina's Customer Service Team
After submitting the prior authorization form, healthcare providers should follow up with Molina's customer service team to ensure that the request has been received and is being processed. This can help resolve any issues or discrepancies that may arise during the review process.

Benefits of Efficient Prior Authorization
Efficient prior authorization can have numerous benefits for healthcare providers, patients, and payers. Some of these benefits include:
- Reduced administrative burdens and costs
- Improved patient outcomes and satisfaction
- Enhanced care coordination and collaboration
- Better management of healthcare resources and utilization
Common Challenges and Solutions
Despite the importance of prior authorization, healthcare providers often face challenges during the process. Some common challenges and solutions include:
- Delays in processing and approval: Use Molina's online prior authorization portal to expedite the process.
- Incomplete or inaccurate forms: Double-check the form for completeness and accuracy before submission.
- Lack of supporting documentation: Ensure that all relevant documentation is attached to the form.

Conclusion
Filling out the Molina prior authorization form requires attention to detail, accuracy, and completeness. By understanding the key components of the form, gathering necessary information and documentation, and following the five ways outlined in this article, healthcare providers can simplify the process and increase the chances of successful authorization.
We encourage healthcare providers to share their experiences and tips for navigating the prior authorization process. Your feedback and insights can help improve the overall quality of care and patient outcomes.
What is the purpose of the Molina prior authorization form?
+The Molina prior authorization form is used to obtain approval for specific medical treatments or services, ensuring that members receive necessary and cost-effective care.
What information is required on the Molina prior authorization form?
+The form requires patient demographics and insurance information, diagnosis and medical history, proposed treatment or medication, clinical rationale and supporting documentation, and healthcare provider's signature and contact information.
How can I expedite the prior authorization process?
+Using Molina's online prior authorization portal can help expedite the process. Additionally, ensuring that the form is complete and accurate, and following up with Molina's customer service team can also help resolve any issues or discrepancies.