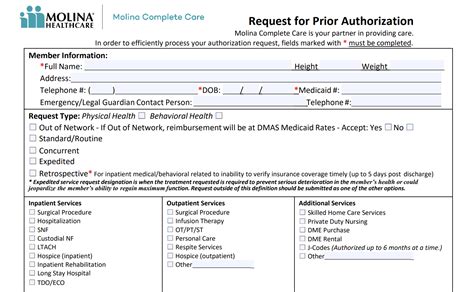
Simplifying the Molina prior authorization form is a crucial step in streamlining healthcare administrative tasks, reducing paperwork, and enhancing the overall efficiency of medical offices. Prior authorizations (PAs) are a mandatory process for healthcare providers to obtain approval from insurance companies before administering specific treatments, medications, or medical procedures. However, the complexity of these forms can lead to significant delays and increased administrative burdens. Here are five strategies to simplify the Molina prior auth form, making the process more manageable for healthcare providers and staff.
Understanding the Importance of Simplification

Prior authorization forms, including those from Molina, often require detailed patient information, treatment plans, and medical justification. The complexity of these forms can lead to increased time spent on paperwork, potential errors, and delays in patient care. By simplifying these forms, healthcare providers can reduce administrative burdens, improve patient satisfaction, and enhance the overall quality of care.
1. Streamline Patient Information
Gathering and Organizing Patient Data
One of the primary challenges in completing prior authorization forms is collecting and organizing patient information. To simplify this process, healthcare providers can implement the following strategies:
- Implement Electronic Health Records (EHRs): EHRs can significantly reduce the time spent on gathering patient information. By having all patient data in one place, healthcare providers can quickly access and populate the necessary fields in the prior authorization form.
- Use Patient Portals: Patient portals can enable patients to provide and update their information electronically, reducing the administrative burden on healthcare staff.
- Develop a Template: Create a template with common patient information fields to help streamline the data collection process.
2. Standardize Medical Justification
Clear and Concise Medical Rationale
Providing clear and concise medical justification is crucial for successful prior authorization. To simplify this process:
- Develop a Library of Pre-Approved Justifications: Create a library of pre-approved medical justifications for common treatments and procedures. This can help reduce the time spent on writing and reviewing justifications.
- Use Evidence-Based Guidelines: Use evidence-based guidelines to support medical justifications, reducing the need for lengthy explanations.
- Collaborate with Providers: Encourage providers to work together to develop standardized justifications for common treatments.
3. Automate Form Completion
Leveraging Technology for Efficiency
Technology can significantly simplify the prior authorization form completion process. Consider the following strategies:
- Prior Authorization Software: Utilize software specifically designed for prior authorization to automate form completion, track submissions, and receive notifications.
- Integrate with EHRs: Integrate prior authorization software with EHRs to streamline data transfer and reduce errors.
- Rules-Based Engines: Implement rules-based engines to automatically populate forms with relevant patient information and medical justification.
4. Reduce Administrative Burden
Minimizing Administrative Tasks
To further simplify the prior authorization form process:
- Designate a Prior Authorization Coordinator: Assign a specific staff member to handle prior authorizations, reducing the administrative burden on providers and other staff.
- Develop a Prior Authorization Checklist: Create a checklist to ensure all necessary information and documentation are included, reducing errors and resubmissions.
- Implement a Prior Authorization Dashboard: Utilize a dashboard to track and monitor prior authorization submissions, approvals, and denials.
5. Optimize Communication
Effective Communication with Molina
Effective communication with Molina is crucial for successful prior authorization. To simplify this process:
- Establish a Single Point of Contact: Designate a single point of contact for prior authorization communication with Molina, reducing confusion and miscommunication.
- Utilize Online Portals: Leverage Molina's online portals to submit prior authorization requests, reducing paperwork and increasing efficiency.
- Regularly Review and Update Information: Regularly review and update patient information and medical justification to ensure accuracy and reduce errors.
Putting it All Together
Simplifying the Molina prior auth form requires a multi-faceted approach that incorporates technology, process optimization, and effective communication. By implementing these strategies, healthcare providers can reduce administrative burdens, improve patient satisfaction, and enhance the overall quality of care.
What's Next?
We would love to hear about your experiences with simplifying prior authorization forms. Share your thoughts, strategies, and challenges in the comments below. Let's work together to make healthcare administration more efficient and patient-centered.
Frequently Asked Questions
What is the purpose of prior authorization?
+Prior authorization is a process that requires healthcare providers to obtain approval from insurance companies before administering specific treatments, medications, or medical procedures.
How can I simplify the prior authorization form process?
+Implement electronic health records, develop a library of pre-approved justifications, automate form completion, reduce administrative burden, and optimize communication with insurance companies.
What are the benefits of simplifying prior authorization forms?
+Reduced administrative burdens, improved patient satisfaction, enhanced quality of care, and increased efficiency in healthcare administration.