The complexities of pharmacy prior authorization can be overwhelming for patients, physicians, and pharmacists alike. With the rise of medication prices and healthcare regulations, pharmacies like Molina Pharmacy are working hard to streamline the process. In this article, we will break down the Molina Pharmacy prior authorization process into 5 easy steps, making it more manageable for all parties involved.
Pharmacy prior authorization is a crucial step in ensuring that patients receive the necessary medications while controlling healthcare costs. However, the process can be time-consuming and bureaucratic, leading to frustration and delays. By understanding the Molina Pharmacy prior authorization process, patients and healthcare providers can better navigate the system and ensure timely access to medications.
To improve patient outcomes and simplify the process, Molina Pharmacy has implemented a user-friendly prior authorization system. By following these 5 steps, patients and healthcare providers can easily initiate and track prior authorization requests, reducing the administrative burden and getting patients the medications they need faster.
Step 1: Verify Patient Eligibility

Before initiating the prior authorization process, it's essential to verify the patient's eligibility. This involves checking the patient's insurance coverage and verifying their membership with Molina Pharmacy. Patients can check their eligibility by logging into their Molina Pharmacy account or contacting their insurance provider directly.
Patient Eligibility Requirements
- Active Molina Pharmacy membership
- Valid insurance coverage
- Up-to-date patient information
Step 2: Gather Required Information

To initiate the prior authorization process, patients and healthcare providers must gather the required information. This includes:
- Patient demographics and contact information
- Prescription details, including medication name, dosage, and frequency
- Medical records and relevant test results
- Physician's order and signature
Required Documents
- Prescription order
- Medical records
- Test results
- Physician's statement
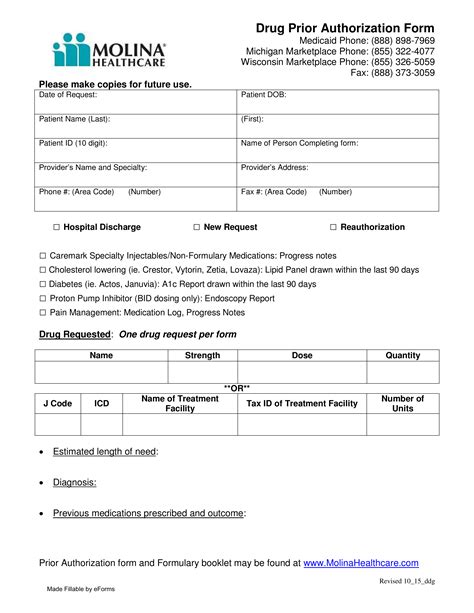
Step 3: Submit the Prior Authorization Request

Once the required information is gathered, the prior authorization request can be submitted to Molina Pharmacy. This can be done online, by phone, or by fax. Patients and healthcare providers can use the Molina Pharmacy prior authorization form to ensure all necessary information is included.
Prior Authorization Submission Options
- Online submission through the Molina Pharmacy portal
- Phone submission by calling the Molina Pharmacy customer service
- Fax submission using the prior authorization form
Step 4: Track the Prior Authorization Status

After submitting the prior authorization request, patients and healthcare providers can track the status online or by contacting Molina Pharmacy customer service. This allows them to stay informed about the progress of the request and ensure timely follow-up.
Prior Authorization Status Updates
- Online tracking through the Molina Pharmacy portal
- Phone updates by calling the Molina Pharmacy customer service
- Email notifications for status changes
Step 5: Receive Prior Authorization Approval or Denial

Once the prior authorization request is reviewed, Molina Pharmacy will notify the patient and healthcare provider of the approval or denial. If approved, the patient can pick up their medication at their local pharmacy. If denied, the patient and healthcare provider can appeal the decision or explore alternative treatment options.
Prior Authorization Outcomes
- Approval with medication coverage
- Denial with explanation and appeal options
- Alternative treatment options
By following these 5 steps, patients and healthcare providers can navigate the Molina Pharmacy prior authorization process with ease. By streamlining the process, Molina Pharmacy aims to improve patient outcomes and reduce the administrative burden associated with prior authorization.
What is prior authorization, and why is it necessary?
+Prior authorization is a process used by insurance companies to review and approve medication requests before dispensing. It's necessary to ensure that patients receive necessary medications while controlling healthcare costs.
How long does the prior authorization process take?
+The prior authorization process typically takes 24-48 hours, but may vary depending on the complexity of the request and the availability of required information.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you and your healthcare provider can appeal the decision or explore alternative treatment options. Molina Pharmacy will provide an explanation for the denial and information on the appeal process.
We hope this article has provided valuable insights into the Molina Pharmacy prior authorization process. By understanding the steps involved, patients and healthcare providers can better navigate the system and ensure timely access to medications. If you have any further questions or concerns, please don't hesitate to reach out to us.