The Ohio Medicaid program, also known as Buckeye Medicaid, provides essential healthcare services to eligible individuals and families. However, to ensure that patients receive necessary treatments and medications while controlling costs, the program requires prior authorization for certain medical procedures and prescriptions. In this article, we will delve into the world of Buckeye Medicaid prior authorization forms, providing you with valuable insights and practical tips to streamline the process.
Understanding the Prior Authorization Process
Before we dive into the tips, it's essential to understand the prior authorization process. Prior authorization is a process used by health insurance companies, including Medicaid, to determine whether a specific treatment, medication, or medical service is medically necessary and covered under the patient's insurance plan. The process involves submitting a prior authorization request to the insurance company, which reviews the request and makes a determination based on the patient's medical needs and the insurance plan's coverage rules.
Tip 1: Familiarize Yourself with the Prior Authorization Form

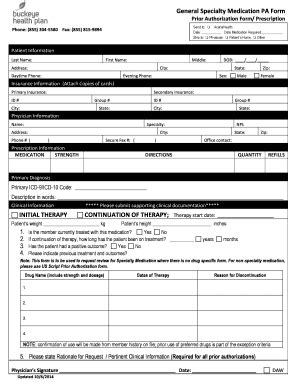
The Buckeye Medicaid prior authorization form is the foundation of the prior authorization process. It's crucial to familiarize yourself with the form's requirements, including the necessary information and documentation needed to support the request. You can find the form on the Ohio Medicaid website or by contacting your local Medicaid office.
What to Include in the Prior Authorization Form
When completing the prior authorization form, make sure to include the following information:
- Patient's demographic information, including name, date of birth, and Medicaid ID number
- Prescriber's information, including name, address, and contact information
- Medical service or prescription being requested
- Diagnosis and medical necessity for the requested service or medication
- Supporting documentation, such as medical records and test results
Tip 2: Ensure Accurate and Complete Information
Accurate and complete information is vital to a successful prior authorization request. Double-check the form for errors and ensure that all required fields are completed. Incomplete or inaccurate information can lead to delays or denials.
Common Mistakes to Avoid
- Incomplete or missing patient demographic information
- Incorrect prescriber information
- Insufficient supporting documentation
- Failure to indicate medical necessity
Tip 3: Submit the Request Electronically
Ohio Medicaid offers an electronic prior authorization submission process, which can expedite the review and determination process. The electronic submission process allows you to submit the request online, reducing the need for paper forms and mail.
Benefits of Electronic Submission
- Faster review and determination process
- Reduced risk of lost or misplaced requests
- Increased accuracy and reduced errors
Tip 4: Follow Up on the Status of Your Request
After submitting the prior authorization request, it's essential to follow up on the status of your request. You can check the status online or by contacting the Ohio Medicaid prior authorization department.
How to Check the Status of Your Request
- Online: Visit the Ohio Medicaid website and log in to your account to check the status of your request.
- Phone: Contact the Ohio Medicaid prior authorization department to inquire about the status of your request.
Tip 5: Be Prepared to Appeal a Denial
If your prior authorization request is denied, don't give up. You have the right to appeal the decision. Be prepared to provide additional information or documentation to support your appeal.
Appeal Process
- Review the denial letter and understand the reason for the denial
- Gather additional information or documentation to support your appeal
- Submit the appeal request online or by mail
- Follow up on the status of your appeal
Conclusion
The Buckeye Medicaid prior authorization form is an essential tool for ensuring that patients receive necessary medical services and prescriptions. By familiarizing yourself with the form, ensuring accurate and complete information, submitting the request electronically, following up on the status of your request, and being prepared to appeal a denial, you can streamline the prior authorization process and improve patient outcomes.
Share Your Experience
Have you experienced challenges with the Buckeye Medicaid prior authorization process? Share your experience and tips in the comments below. Your insights can help others navigate the process and improve patient care.
FAQ Section
What is the purpose of the Buckeye Medicaid prior authorization form?
+The Buckeye Medicaid prior authorization form is used to determine whether a specific treatment, medication, or medical service is medically necessary and covered under the patient's insurance plan.
How do I submit a prior authorization request electronically?
+You can submit a prior authorization request electronically through the Ohio Medicaid website. Simply log in to your account and follow the prompts to submit your request.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you have the right to appeal the decision. Gather additional information or documentation to support your appeal and submit the appeal request online or by mail.