Understanding the Importance of the Molina Appeal Form in Ohio

In Ohio, the Molina appeal form is a crucial document for individuals who have been denied coverage or benefits by Molina Healthcare, a leading healthcare provider in the state. The form serves as a platform for beneficiaries to contest the decision and advocate for their rights. With the rising cost of healthcare, it's essential to understand the importance of completing the Molina appeal form accurately to ensure a successful outcome.
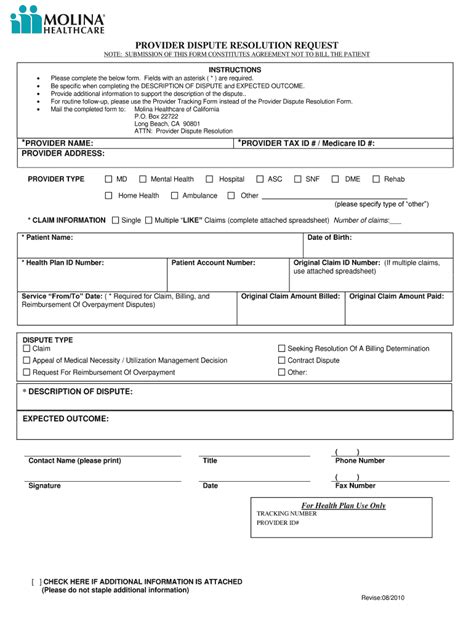
The Role of the Molina Appeal Form in Resolving Disputes

The Molina appeal form plays a vital role in resolving disputes between beneficiaries and Molina Healthcare. By submitting the form, individuals can request a review of the initial decision, providing an opportunity to present new evidence or clarify existing information. This process ensures that beneficiaries receive fair and impartial treatment, ultimately leading to a more satisfying outcome.
5 Ways to Complete the Molina Appeal Form in Ohio

Completing the Molina appeal form in Ohio requires attention to detail and a thorough understanding of the process. Here are five ways to ensure a successful submission:
1. Gather Required Documents
Before starting the appeal process, gather all necessary documents, including:
- The original denial letter from Molina Healthcare
- Relevant medical records and test results
- Supporting documentation, such as letters from healthcare providers or proof of income
- A copy of the beneficiary's identification and insurance card
2. Understand the Appeal Process
Familiarize yourself with the appeal process and timeline. In Ohio, beneficiaries have 60 days from the date of the denial letter to submit the appeal form. It's essential to understand the different levels of appeal, including:
- Level 1: Initial Review
- Level 2: Reconsideration
- Level 3: External Review
3. Complete the Appeal Form Accurately
Fill out the Molina appeal form accurately and thoroughly. Ensure that all required fields are completed, and any additional information is provided in the designated spaces. Make sure to:
- Sign and date the form
- Provide a clear and concise statement explaining the reason for the appeal
- Attach all supporting documentation
4. Submit the Appeal Form
Submit the completed appeal form to Molina Healthcare via mail, fax, or online portal. Ensure that the form is received within the 60-day timeframe. If submitting by mail, use certified mail with return receipt requested to track the delivery.
5. Follow Up on the Appeal Status
After submitting the appeal form, follow up on the status of the appeal. Contact Molina Healthcare's customer service department to confirm receipt of the form and to inquire about the expected timeline for a decision.
Additional Tips and Considerations
- Keep a record of all correspondence and communication with Molina Healthcare.
- Ensure that all documentation is organized and easily accessible.
- If necessary, consider seeking assistance from a patient advocate or attorney.
Conclusion: Empowering Beneficiaries through Knowledge

By understanding the importance of the Molina appeal form and following the steps outlined above, beneficiaries in Ohio can effectively navigate the appeal process. Empowering individuals with knowledge and resources ensures that they receive the care and benefits they deserve.
A Final Note: Taking Action

Don't let a denied claim or benefit decision go unchallenged. Take action today by completing the Molina appeal form and advocating for your rights. Share this article with others who may be facing similar challenges, and together, let's empower the community to take control of their healthcare.
FAQ Section:
What is the deadline for submitting the Molina appeal form in Ohio?
+Beneficiaries have 60 days from the date of the denial letter to submit the appeal form.
Can I submit the Molina appeal form online?
+Yes, beneficiaries can submit the appeal form online through Molina Healthcare's website.
What documentation is required to support my appeal?
+Required documentation may include medical records, test results, and supporting letters from healthcare providers.