The process of obtaining prior authorization for medications can be a daunting task for healthcare providers and patients alike. Southern Scripts, a pharmacy benefit management company, requires a prior authorization form to be completed before approving certain medications. In this article, we will guide you through the process of completing a Southern Scripts prior authorization form, highlighting the importance of prior authorization, the benefits of using Southern Scripts, and providing tips for a successful submission.
Understanding Prior Authorization
Prior authorization is a process used by health insurance companies and pharmacy benefit management companies to ensure that certain medications are medically necessary and cost-effective. The process involves a healthcare provider submitting a request for approval before prescribing a specific medication. This helps to prevent unnecessary costs and ensures that patients receive the most effective treatment.
Benefits of Using Southern Scripts
Southern Scripts is a leading pharmacy benefit management company that offers a range of services, including prior authorization. By using Southern Scripts, healthcare providers can benefit from:
- Streamlined prior authorization process
- Access to a comprehensive formulary
- Personalized customer support
- Cost-effective medication management
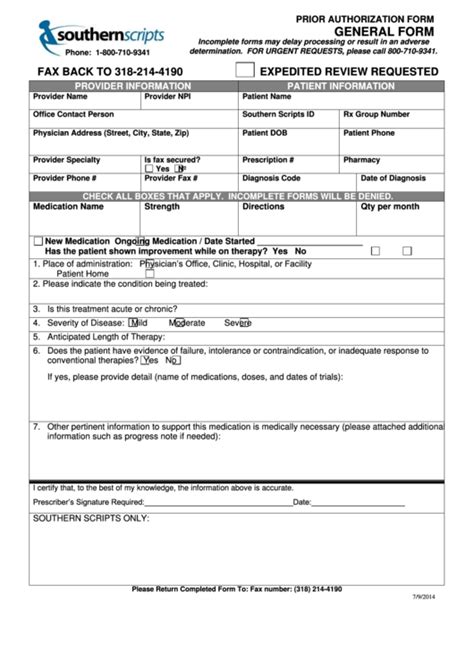
Completing a Southern Scripts Prior Authorization Form
Completing a Southern Scripts prior authorization form requires careful attention to detail and accurate information. Here's a step-by-step guide to help you through the process:

- Patient Information: Start by providing the patient's demographic information, including name, date of birth, and contact details.
- Medication Information: Clearly state the medication being requested, including the name, strength, and dosage.
- Diagnosis: Provide a clear diagnosis and medical justification for the requested medication.
- Clinical Information: Include relevant clinical information, such as medical history, test results, and previous treatments.
- Prescriber Information: Provide the prescriber's name, contact details, and licensure information.
- Supporting Documentation: Attach any supporting documentation, such as lab results, medical records, or specialist reports.
Tips for a Successful Submission
To ensure a successful submission, follow these tips:
- Complete the form accurately: Double-check the form for errors or omissions.
- Provide clear documentation: Ensure that all supporting documentation is clear and legible.
- Submit the form promptly: Submit the form in a timely manner to avoid delays.
- Follow up: Follow up with Southern Scripts to ensure that the form has been received and is being processed.
Southern Scripts Prior Authorization Form Requirements
Southern Scripts has specific requirements for prior authorization forms. Here are some key requirements:
- Form must be completed in its entirety: All sections of the form must be completed accurately and thoroughly.
- Form must be signed and dated: The form must be signed and dated by the prescriber.
- Supporting documentation must be attached: All relevant supporting documentation must be attached to the form.
Common Reasons for Prior Authorization Denials
Prior authorization requests can be denied for a variety of reasons. Here are some common reasons:
- Incomplete or inaccurate form: The form is incomplete or contains errors.
- Lack of supporting documentation: Insufficient or missing supporting documentation.
- Medication not medically necessary: The medication is not deemed medically necessary.
Appealing a Prior Authorization Denial
If a prior authorization request is denied, you can appeal the decision. Here's how:
- Submit a written appeal: Submit a written appeal to Southern Scripts, stating the reason for the appeal.
- Provide additional information: Provide additional information or supporting documentation to support the appeal.
- Follow up: Follow up with Southern Scripts to ensure that the appeal is being processed.

Conclusion
Completing a Southern Scripts prior authorization form requires attention to detail and accurate information. By following the tips and guidelines outlined in this article, you can ensure a successful submission and avoid common mistakes. Remember to appeal any denied requests and follow up with Southern Scripts to ensure that your patients receive the necessary medications.
Take Action
If you have any questions or concerns about the prior authorization process, contact Southern Scripts customer support. Don't hesitate to reach out to us if you need help with completing a prior authorization form or appealing a denied request.
Share Your Thoughts
Have you had any experiences with prior authorization forms or appeals? Share your thoughts and comments below.
FAQ Section
What is prior authorization?
+Prior authorization is a process used by health insurance companies and pharmacy benefit management companies to ensure that certain medications are medically necessary and cost-effective.
Why do I need to complete a prior authorization form?
+You need to complete a prior authorization form to ensure that the medication being requested is medically necessary and cost-effective.
How long does it take to process a prior authorization request?
+The processing time for a prior authorization request varies, but it typically takes 24-48 hours.