The Medicare claim process can be complex and time-consuming, especially when it comes to filling out forms. One of the most important forms for healthcare providers to complete is the CMS-1490S, also known as the Medicare Crossover Claims Form. This form is used to request payment from Medicare for services rendered to Medicare beneficiaries who also have other insurance coverage. In this article, we will provide five tips for completing Medicare Form CMS-1490S accurately and efficiently.
Understanding the CMS-1490S Form

The CMS-1490S form is used to request payment from Medicare for services rendered to Medicare beneficiaries who have other insurance coverage, such as Medicaid or private insurance. The form requires providers to submit claims for Medicare crossover claims, which are claims that have already been paid by another insurance carrier.
Tip 1: Ensure Accurate Patient Information
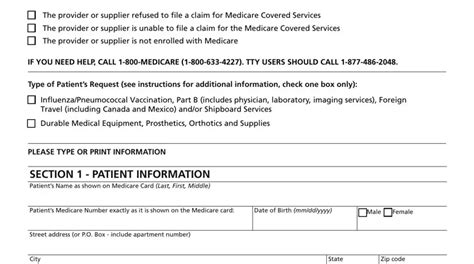
The first tip for completing the CMS-1490S form is to ensure that the patient's information is accurate. This includes the patient's name, date of birth, and Medicare identification number. Providers should verify this information with the patient or their representative to ensure that it is correct.
Tip 2: Determine the Correct Claim Type
The CMS-1490S form requires providers to determine the correct claim type. There are two types of claims: institutional and professional. Institutional claims are for services rendered in a hospital or other institutional setting, while professional claims are for services rendered by a physician or other healthcare professional. Providers should ensure that they select the correct claim type to avoid delays in processing.
Tip 3: Complete the Form in its Entirety
The CMS-1490S form requires providers to complete all fields, including the claimant's name and address, the patient's name and address, and the services rendered. Providers should ensure that all fields are completed accurately and thoroughly to avoid delays in processing.
Tip 4: Attach Supporting Documentation
The CMS-1490S form requires providers to attach supporting documentation, such as the Explanation of Benefits (EOB) from the other insurance carrier. Providers should ensure that all supporting documentation is attached to the form to avoid delays in processing.
Tip 5: Submit the Form Electronically
The final tip for completing the CMS-1490S form is to submit it electronically. The Centers for Medicare and Medicaid Services (CMS) encourages providers to submit claims electronically through the Medicare Administrative Contractor (MAC) website. Electronic submission can help to reduce errors and improve processing time.
Common Errors to Avoid

When completing the CMS-1490S form, there are several common errors to avoid. These include:
- Incomplete or inaccurate patient information
- Incorrect claim type
- Missing or incomplete supporting documentation
- Failure to submit the form electronically
By avoiding these common errors, providers can help to ensure that their claims are processed efficiently and accurately.
Best Practices for Completing the CMS-1490S Form

To ensure that the CMS-1490S form is completed accurately and efficiently, providers should follow best practices. These include:
- Verifying patient information with the patient or their representative
- Using a checklist to ensure that all fields are completed accurately and thoroughly
- Attaching all supporting documentation, including the EOB from the other insurance carrier
- Submitting the form electronically through the MAC website
By following these best practices, providers can help to ensure that their claims are processed efficiently and accurately.
Conclusion

Completing the CMS-1490S form can be a complex and time-consuming process, but by following the tips and best practices outlined in this article, providers can help to ensure that their claims are processed efficiently and accurately. By verifying patient information, determining the correct claim type, completing the form in its entirety, attaching supporting documentation, and submitting the form electronically, providers can help to avoid common errors and ensure that their claims are processed correctly.
We invite you to share your thoughts and experiences with completing the CMS-1490S form in the comments below. Have you encountered any challenges or errors when completing this form? How have you overcome these challenges? Share your insights and best practices with us!
What is the purpose of the CMS-1490S form?
+The CMS-1490S form is used to request payment from Medicare for services rendered to Medicare beneficiaries who have other insurance coverage.
What type of claims can be submitted using the CMS-1490S form?
+The CMS-1490S form can be used to submit institutional and professional claims for services rendered to Medicare beneficiaries who have other insurance coverage.
What documentation is required to be attached to the CMS-1490S form?
+The CMS-1490S form requires providers to attach supporting documentation, including the Explanation of Benefits (EOB) from the other insurance carrier.