The prior authorization process can be a complex and time-consuming task for healthcare providers, patients, and pharmacists. The IngenioRx prior authorization form is a crucial document that plays a significant role in ensuring that patients receive the necessary medications while controlling healthcare costs. In this article, we will provide a comprehensive guide to the IngenioRx prior authorization form, its benefits, and the steps involved in the process.
Understanding the IngenioRx Prior Authorization Form

The IngenioRx prior authorization form is a document required by IngenioRx, a pharmacy benefit management (PBM) company, to ensure that certain medications are medically necessary and cost-effective. The form is typically completed by the healthcare provider and submitted to IngenioRx for review. The prior authorization process helps to:
- Ensure that patients receive the most effective and safe treatment options
- Control healthcare costs by preventing unnecessary or duplicate prescriptions
- Promote the use of generic or alternative medications when possible
- Enhance patient safety by monitoring potential medication interactions or side effects
Benefits of the IngenioRx Prior Authorization Form
The IngenioRx prior authorization form offers several benefits to patients, healthcare providers, and payers. Some of the key benefits include:
- Improved patient outcomes: By ensuring that patients receive the most effective and safe treatment options, the prior authorization process can lead to better health outcomes.
- Cost savings: The prior authorization process helps to control healthcare costs by preventing unnecessary or duplicate prescriptions.
- Enhanced patient safety: The prior authorization process helps to monitor potential medication interactions or side effects, promoting patient safety.
- Streamlined process: The IngenioRx prior authorization form simplifies the prior authorization process, reducing administrative burdens on healthcare providers and pharmacists.
Steps Involved in the IngenioRx Prior Authorization Process

The IngenioRx prior authorization process involves several steps:
- Prescription: The healthcare provider prescribes a medication to the patient.
- Prior Authorization Request: The pharmacist or healthcare provider submits a prior authorization request to IngenioRx, including the completed IngenioRx prior authorization form.
- Review: IngenioRx reviews the prior authorization request to determine if the medication is medically necessary and cost-effective.
- Approval or Denial: IngenioRx approves or denies the prior authorization request, providing a detailed explanation for the decision.
- Appeal: If the prior authorization request is denied, the healthcare provider or patient can appeal the decision.
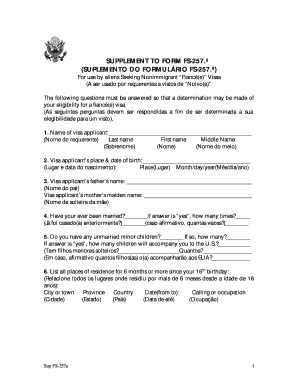
Required Information for the IngenioRx Prior Authorization Form
The IngenioRx prior authorization form requires the following information:
- Patient demographics
- Medication information, including the prescribed medication and dosage
- Medical condition or diagnosis
- Treatment history and previous medications
- Healthcare provider information, including name and contact details
Common Challenges and Solutions

The IngenioRx prior authorization process can be complex and time-consuming, leading to several challenges. Some common challenges and solutions include:
- Delays in approval: To minimize delays, healthcare providers can submit prior authorization requests electronically or via fax.
- Denials: To reduce denials, healthcare providers can ensure that the prior authorization form is completed accurately and includes all required information.
- Administrative burdens: To streamline the process, healthcare providers can use online portals or software to manage prior authorization requests.
Best Practices for Submitting the IngenioRx Prior Authorization Form

To ensure a smooth prior authorization process, healthcare providers can follow these best practices:
- Complete the form accurately: Ensure that all required information is included and accurate.
- Submit the form electronically: Submit the prior authorization form electronically or via fax to minimize delays.
- Include supporting documentation: Provide supporting documentation, such as medical records or test results, to support the prior authorization request.
- Follow up: Follow up with IngenioRx to ensure that the prior authorization request is processed in a timely manner.
Conclusion

The IngenioRx prior authorization form is a crucial document that plays a significant role in ensuring that patients receive the necessary medications while controlling healthcare costs. By understanding the benefits and steps involved in the prior authorization process, healthcare providers can streamline the process and improve patient outcomes. By following best practices and submitting the form accurately, healthcare providers can minimize delays and denials, promoting a more efficient prior authorization process.
We hope this comprehensive guide has provided valuable insights into the IngenioRx prior authorization form. If you have any questions or concerns, please leave a comment below or share this article with your colleagues.
What is the IngenioRx prior authorization form?
+The IngenioRx prior authorization form is a document required by IngenioRx, a pharmacy benefit management (PBM) company, to ensure that certain medications are medically necessary and cost-effective.
What information is required for the IngenioRx prior authorization form?
+The IngenioRx prior authorization form requires patient demographics, medication information, medical condition or diagnosis, treatment history and previous medications, and healthcare provider information.
How can I minimize delays in the prior authorization process?
+To minimize delays, healthcare providers can submit prior authorization requests electronically or via fax, and ensure that the form is completed accurately and includes all required information.