Understanding Highmark Outpatient Authorization: A Comprehensive Guide

Highmark outpatient authorization is a process that healthcare providers and patients must navigate to obtain approval for medical treatments and services. This process can be complex and time-consuming, but understanding the steps involved can help streamline the experience. In this article, we will break down the Highmark outpatient authorization process into five easy steps, providing a comprehensive guide for healthcare providers and patients.
The Importance of Outpatient Authorization
Outpatient authorization is a critical step in ensuring that patients receive the necessary medical care while also controlling healthcare costs. By obtaining prior approval for medical treatments and services, healthcare providers can avoid unnecessary procedures and reduce the financial burden on patients. Highmark, a leading health insurance provider, requires outpatient authorization for certain medical services to ensure that patients receive high-quality, cost-effective care.
Step 1: Verify Patient Eligibility

The first step in the Highmark outpatient authorization process is to verify patient eligibility. Healthcare providers must check the patient's insurance coverage and ensure that they are eligible for the requested medical service. This involves verifying the patient's policy details, including their coverage dates, deductibles, and copays. Providers can use Highmark's online portal or contact their customer service department to verify patient eligibility.
Step 1 Benefits: Efficient Claims Processing
Verifying patient eligibility upfront helps prevent claim denials and reduces the administrative burden on healthcare providers. By ensuring that patients are eligible for the requested medical service, providers can avoid unnecessary paperwork and focus on delivering high-quality care.
Step 2: Determine Medical Necessity

The second step in the Highmark outpatient authorization process is to determine medical necessity. Healthcare providers must assess the patient's medical condition and determine whether the requested medical service is medically necessary. This involves evaluating the patient's symptoms, medical history, and treatment options to ensure that the requested service is the most appropriate course of treatment.
Step 2 Benefits: Reduced Healthcare Costs
Determining medical necessity helps reduce healthcare costs by ensuring that patients receive only the necessary medical services. By evaluating the patient's medical condition and treatment options, providers can avoid unnecessary procedures and reduce the financial burden on patients.
Step 3: Gather Required Documentation

The third step in the Highmark outpatient authorization process is to gather required documentation. Healthcare providers must collect all necessary documents, including medical records, test results, and treatment plans, to support the requested medical service. This documentation must be complete and accurate to ensure that the authorization request is processed efficiently.
Step 3 Benefits: Faster Authorization Processing
Gathering required documentation upfront helps streamline the authorization process and reduces the risk of delays. By providing complete and accurate documentation, providers can ensure that their authorization requests are processed quickly and efficiently.
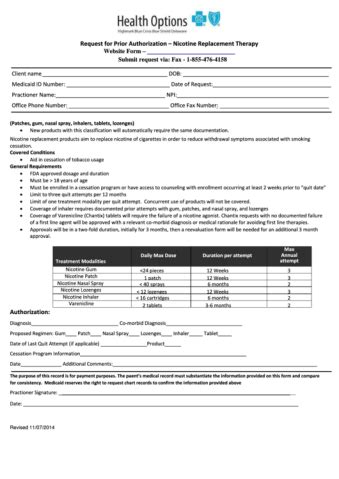
Step 4: Submit Authorization Request

The fourth step in the Highmark outpatient authorization process is to submit the authorization request. Healthcare providers must submit the completed authorization request form, along with the required documentation, to Highmark for review. Providers can submit the request online, by phone, or by mail, depending on their preference.
Step 4 Benefits: Convenient Submission Options
Submitting the authorization request is a convenient process, with multiple submission options available. Providers can choose the method that works best for them, whether it's online, by phone, or by mail.
Step 5: Receive Authorization Determination

The final step in the Highmark outpatient authorization process is to receive the authorization determination. Highmark will review the authorization request and make a determination based on the patient's medical condition and treatment options. Providers will receive notification of the determination, which may include approval, denial, or additional information requests.
Step 5 Benefits: Clear Communication
Receiving the authorization determination provides clear communication about the patient's coverage and treatment options. Providers can use this information to inform their patients and make informed decisions about their care.
Conclusion
The Highmark outpatient authorization process may seem complex, but breaking it down into five easy steps can help streamline the experience. By verifying patient eligibility, determining medical necessity, gathering required documentation, submitting the authorization request, and receiving the authorization determination, healthcare providers can ensure that their patients receive the necessary medical care while also controlling healthcare costs.Call to Action
We encourage healthcare providers and patients to share their experiences with the Highmark outpatient authorization process. Your feedback can help us improve our services and provide better support to our customers. Leave a comment below or share this article with your network to help us spread the word.What is Highmark outpatient authorization?
+Highmark outpatient authorization is a process that healthcare providers and patients must navigate to obtain approval for medical treatments and services.
How do I verify patient eligibility?
+Healthcare providers can verify patient eligibility by checking the patient's insurance coverage and ensuring that they are eligible for the requested medical service. This can be done online or by contacting Highmark's customer service department.
What documentation is required for Highmark outpatient authorization?
+Healthcare providers must collect all necessary documents, including medical records, test results, and treatment plans, to support the requested medical service.