As a healthcare provider, navigating the complexities of prior authorization forms can be overwhelming. One of the most widely used forms is the Highmark Prior Authorization Form. In this article, we'll break down the key aspects of this form, providing you with a simplified guide to make the process smoother.
Prior authorization is a critical step in the healthcare process, ensuring that patients receive necessary treatments while controlling healthcare costs. Highmark, a leading health insurance company, requires healthcare providers to submit a prior authorization form to determine the medical necessity of certain treatments or services. This form helps Highmark make informed decisions about coverage, reducing the risk of denied claims and delayed care.
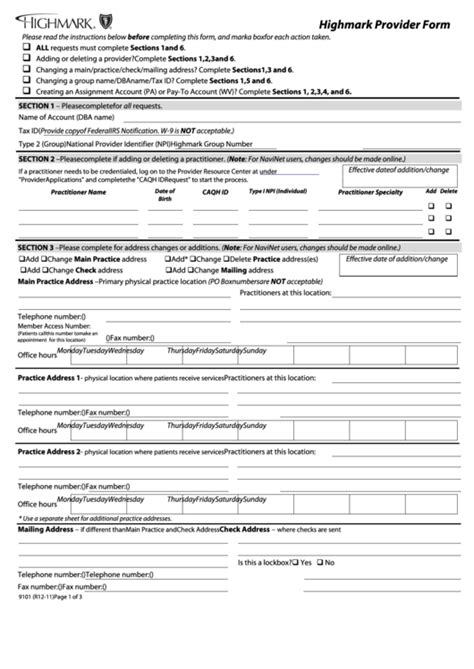
Understanding the Highmark Prior Authorization Form
The Highmark Prior Authorization Form is a standardized document used to request pre-approval for specific medical services, treatments, or prescriptions. The form typically includes the following sections:
- Patient demographics and insurance information
- Treatment or service details, including diagnosis and procedure codes
- Clinical information, such as medical history and current treatment plans
- Supporting documentation, including lab results and medical records
Step-by-Step Guide to Completing the Form
- Patient Information: Begin by filling out the patient's demographic information, including name, date of birth, and insurance ID number.
- Treatment or Service Details: Clearly specify the treatment or service being requested, including the procedure code and diagnosis code.
- Clinical Information: Provide a detailed clinical summary, including the patient's medical history, current treatment plans, and any relevant lab results or medical records.
- Supporting Documentation: Attach all relevant supporting documentation, such as lab results, medical records, and consultation reports.
- Provider Information: Complete the provider section, including your name, title, and contact information.

Tips for Streamlining the Process
- Ensure all required fields are completed accurately and thoroughly.
- Use standardized diagnosis and procedure codes to avoid delays.
- Attach all supporting documentation to avoid additional requests for information.
- Submit the form electronically, if possible, to reduce processing time.
Benefits of Prior Authorization
While the prior authorization process may seem burdensome, it offers several benefits, including:
- Reduced denied claims and delayed care
- Improved patient outcomes through timely access to necessary treatments
- Enhanced collaboration between healthcare providers and insurance companies
- More accurate and efficient claims processing
Common Challenges and Solutions
Despite its benefits, the prior authorization process can be challenging. Some common issues and solutions include:
- Incomplete or inaccurate information: Double-check all fields and supporting documentation to ensure accuracy.
- Delayed processing: Submit the form electronically and follow up with Highmark to ensure timely processing.
- Denial of coverage: Review Highmark's coverage policies and resubmit the form with additional supporting documentation, if necessary.

Conclusion and Next Steps
Mastering the Highmark Prior Authorization Form is crucial for healthcare providers seeking to streamline the prior authorization process. By following this simplified guide, you'll be better equipped to navigate the complexities of prior authorization and improve patient outcomes.
If you have any questions or concerns about the prior authorization process, we encourage you to share them in the comments below. Additionally, feel free to share this article with your colleagues and peers to help spread awareness about the importance of prior authorization.
What is the purpose of the Highmark Prior Authorization Form?
+The Highmark Prior Authorization Form is used to request pre-approval for specific medical services, treatments, or prescriptions to determine medical necessity and coverage.
How do I submit the Highmark Prior Authorization Form?
+You can submit the form electronically or by mail, depending on the specific requirements of Highmark and your practice.
What happens if my prior authorization request is denied?
+If your prior authorization request is denied, you can review Highmark's coverage policies and resubmit the form with additional supporting documentation, if necessary.